This page is an open forum for you to share your thoughts with colleagues.
Please consider submitting a brief blog with perspectives about our lives in medicine.
Blog anonymously with minimal descriptive information, or with your name.
Submit to pwp@TCMS.com
Submitted February 2026
by Troy Alexander

Connected in Community
We are all recovering from something.
Maybe you are like me, and recovery comes from childhood trauma.
Maybe you were hurt as an adult.
Maybe you are grieving a loss that still catches you off guard.
Or maybe you are fighting battles with addiction—quiet ones, loud ones, or ones we wish we didn’t have to name.
No matter what it is, you’re not alone.
I serve regularly in a local recovery ministry, and every time I’m there, I’m reminded that healing is not a solo sport. We sit together to share our struggles, celebrate the victories (small or large), and try our best to find healthier rhythms. Different stories. Same need to not be alone.
And that’s where community becomes more than a nice idea -- it becomes essential.
Philosopher Dismas Masolo, in his book Community, Identity, and the Cultural Space, described modern communities as “open ended and amorphous,” defined not by who’s in the room but by what the people in that room believe and practice together. I love that thought–you can be part of many groups, yet only some will feel like home.
Take UT football, for example (Yes, I’m going there). I can sit in the same seats every game, surrounded by the same fans. I don’t really know them, but we do share a similar passion for those few Saturdays every year. We all yell at the same refs and cheer for the same touchdowns. For a few hours, we’re united. But at the end of the day, they don’t know me. This is not a community–it is shared enthusiasm.
Community, however, IS where you can take off the mask, even just a little. That is one of the reasons I believe so deeply in the role of the Travis County Medical Society (TCMS). Physicians spend their days caring for others, often without a place where they can exhale, be human, or admit they need support, too.
TCMS isn’t just an organization, it’s a community designed for physicians to connect, grow, and show up as their real selves. A place where professional development meets personal support. A place where the healer gets to be heard, understood, and known.
Let’s be honest: crossing that threshold into a new group for the first time is uncomfortable. I remember that feeling clearly in my own life—wondering if I’d fit in, if anyone would talk to me, or if I was interrupting some established circle.
But here’s the good news: once you step through the door, connection becomes possible.
Here are a few easy places to start with TCMS:
Join us at the TCMS Installation Dinner on Thursday, February 26th.
Come to the TCM Alliance “Party with a Purpose” in late March.
Watch a summer movie with us—low pressure, easy conversations.
But TCMS isn’t just about social events. It is a lifeline when life gets heavy and you need a little help recovering from your something.
If you’re struggling—whether with burnout, emotional strain, or addiction—our Physician Wellness Program and Physician Health and Rehabilitation Committee (PHRC) are here to walk with you. Quietly. Compassionately. And without judgment.
It all starts with one small action—replying to an email, signing up for dinner, raising your hand in a room where you don’t know everyone yet.
And while I’m at TCMS, I want you to know this: we’ll keep asking what you need, listening to your responses, and building a community that feels less like an institution and more like a home base for Austin physicians.
Because healing happens in community. And you deserve a community that supports your healing, too.
Troy Alexander, CAE
Executive Vice President/CEO – TCMS
tcms@tcms.com
Submitted February 2026
by Dr. Brian Sayers

Three Score and Ten
I turned seventy this week. Most years I do everything I can to ignore my birthday. I tried to do the same this year, but this time it made me pause and consider where I've been and where I hope to go. I have been blessed with a fantastic family, good health, and not too much to worry about. Like love and friendships, I look at my work through a different lens at this point in my life. It is now a privilege, even a pleasure most days to go to work, to be with patients I care about, colleagues I admire, and long-time staff at my office who I can count on. I hope to keep practicing for a few more years, and I will be sad to give it up.
It was the right time to reread Falling Upward by Richard Rohr as my birthday approached. The overall theme of the book is that there are two phases in life. In the first part, we are building and filling our “container.” The container is built and filled with things that we pursue through much of our lives ─ career, relationships, success, and a sense of identity and our place in this world. Importantly, it is also filled with what we accumulate and things that feed our ego. We often feel defined by how the world perceives us. He notes that in the second part of our life journey, we realize that much of what we have filled that container with needs to be emptied and replaced with things that lead to spiritual wholeness, self-discovery, and to lives lived authentically. It is a shift that we drift to, often without realizing it at first. It is time to focus more on things internal than external for the next, definitive phase of life. Life comes in the shape of an arc, he notes. We enter life with nothing but a divine spark. We travel through the wide world exploring, accumulating, finding love, learning from missteps and misfortune, often cluttering our lives with nonsense along the way. We abandon much of this later, now looking inward, hopefully discovering our true self as we return to our simple, sacred essence…and the arc is complete.
At the end of Elizabeth Stout’s Pulitzer Prize winning novel Olive Kitteridge, the main character looks back as she enters her later years, which have become surprisingly rich and full of love after years of loneliness and grief. She reflects on the great lessons she has learned, “…that love was not to be tossed away carelessly as if it were a tart on a platter…” and that at times when her life had been full of love, she “had flicked it off crumbs at a time ... because she had not known what one should know: that day after day was unconsciously squandered.”
Her lesson is a good one—obvious—but usually overlooked as we focus on the small things that fill our days. Each day is to be savored. I realize it more now than I used to. I love my family and my friends, my colleagues, and my patients. Always a little late to figure things out, I realize just how much I love life itself. And goodness… how I love my work.
Brian Sayers, MD
Associate Dean for Curriculum, Dell Medical School
tcms@tcms.com
Submitted January 2026
by Dr. Sherine Salib

Start with the End in Mind
“If a man knows not to which port he sails, no wind is favorable.” ~ Seneca, Stoic Philosopher
Starting with the end in mind is a powerful approach for any career, perhaps even more so for the fast-paced, hectic and ever-changing world of healthcare.
In an exercise used in some company and executive settings, and said to famously have been implemented by Warren Buffet, individuals are encouraged to take time to write their own obituary and then live it backwards. This same sentiment is highlighted in Stephen Covey’s celebrated book The Seven Habits of Highly Effective People— start with the end in mind.
Pausing and reflecting on how we want to be remembered, what our legacy will be when we—and others—look back at our years of work as physicians, is a powerful tool to remind us how we should live our day-to-day work today. This is a humbling and sobering perspective. It is a powerful tool that can help us reverse-engineer our choices and focus on the truly important everyday moments.
Our society tells us to focus inward, to compete, to climb, and to reach for more heights—whatever the cost might be. In the business of healthcare, the hectic pace of patient care, and the competitive nature of academia, this is a reminder to look outward—to focus on others, to contribute, to serve...to make a difference.
We are fortunate that our field of practice—that of medicine, with all its hustle and bustle—affords us more opportunities than most others to serve, and to make a difference.
So, I invite you today to pause with me. To reflect.
What is your personal mission, and how does that align with your day-to-day work in patient care?
When your career is over and you look back, what is the legacy you want to leave behind?
Will you, perhaps, be described as a lifelong learner, or someone whose greatest achievement was not necessarily the professional accolades and accomplishments, but rather the act of always showing up for others?
Will others remember your reputation for compassion and kindness?
What is your personal mission statement, and what are the values that guide that?
When all is said and done, what is the difference you want to make?
Clarity of destination gives every step its purpose.
“To begin with the end in mind means to start with a clear understanding of your destination. It means to know where you’re going so that you better understand where you are now and so that the steps you take are always in the right direction.” - Stephen R. Covey
Sherine Salib, MD, MRCP, FACP
Associate Dean for Curriculum, Dell Medical School
tcms@tcms.com
Submitted January 2026
by Dr. Richard DeBehnke

Welcome Home
Janus was the Roman god of beginnings and endings. He is often recalled at New Year’s, depicted with two faces looking forward and backward. He reflects on what has happened and peers into the future—not as a prophet, but to recognize the significance of transitions.
Last year, the TCMS Physician Wellness Program (PWP) faced its own transition. I want to recognize the hard work of our steering committee members in rising to the occasion and successfully sustaining this important program. Over the past twelve months, we were able to provide over 500 therapy sessions to more than 100 of our colleagues—visits that are anonymous and free.
Our fundraising efforts this year were quite successful, exceeding previous years by more than 18%. Our contributions came from diverse sources, as listed below. Donations from individuals accounted for one third of our total. This grassroots support from our peers is especially touching!
In 2026, we hope to build on our past success and to not only continue the Safe Harbor Counseling Program but grow and expand the role of the PWP in new ways. As we look to the future, we need your support to sustain and grow the program.
Support PWP by continuing the generous financial support that we have received in the past. When you renew your dues, please consider remembering us.
Be an ambassador for the program. Make yourself aware of the services that we offer and have the courage to be the one that reaches out to a colleague in distress, directing them to help.
Attend the CME events we sponsor—these events are all focused on improving physician well-being.
Read our blog weekly. Not only does it contain announcements of CME and other events, it contains our weekly essays. These essays come from you. The care and wisdom that are shared in these contributions are incredibly inspirational.
As well as reading the blog, please consider sharing your thoughts, concerns and insights with us in any medium you choose, whether it be written, drawn or sung. We all underestimate our ability to create and the impact that it can have on our peers.
Perhaps the most important way one can support our program is by utilizing it. I challenge all of you reading this to reflect on your training and your career. I believe that we can all find episodes in our lives where we would have benefited from counseling—sharing our anxiety and fears to become a more complete person.
Our profession is demanding but virtuous. It demands that we try to do the right thing because it is right and not for our personal gain. It helps us live well and find greater meaning in our lives. Our actions can inspire others and have ripple effects that make our community better. But, our profession also requires courage.
Author C.S. Lewis described courage as not one of the virtues, but the form of every virtue at the testing point. We are tested daily, whether by the rigors of our job or by inefficient EMRs, arbitrary metrics, prior authorizations or any of the dozens of hurdles we encounter.
We are the PWP. You are the PWP. And we are here for each other.
Richard DeBehnke, MD
PWP Steering Committee Chair
tcms@tcms.com
Submitted January 2026
by Dr. Blair Walker

Welcome Home
I have been in Travis County—and a member of the Travis County Medical Society—since I was an intern in 2009. At the time, our employer Seton and my Psychiatry Residency Program automatically signed us up every year as a benefit of our employment. It was always there for me, and I eventually started paying the annual dues on my own.
Just over a year ago, during my ninth year as an attending physician after five years in residency training, I received one of those renewal requests and checked some "I Have an Interest In..." boxes for the first time and—BAM! —I was on the Women in Medicine Committee. When I saw that an old buddy from residency, Dr. Holli Sadler, was the new Executive Board president, I figured I’d have a friendly face and checked the box for being an Alternate Delegate and—BAM! —I was signed up for that too! I was later asked—after they got to know me and understood my expertise in Psychiatry and Addiction Medicine—to join the Physician Health Rehabilitation Committee, supporting our colleagues in recovery from substance use disorders—which has been incredibly rewarding and meaningful.
I also heeded the "call to arms" last legislative session and after cajoling some other colleagues to join me, went up to the Capitol after work to testify about the "scope creep" concerns. We sat for several hours watching the dance of politics in the reverential environment of the Senate Chamber and learned from other physicians who clearly do it all of the time. It was fascinating and frankly really cool to be able to help educate our legislators, enacting change at the government level. I hope others will be inspired to get involved in the future, because it is an easy and highly organized First Tuesdays Program, with alerts from TCMS to participate in testimony throughout the session.
Now that I am more involved with TCMS, I can easily say that I feel much more connected to local doctors in our community from many different specialties other than my own, and that I now have a “home” at TCMS. The networking is incredible. At the Annual Awards Dinner, I shook hands with attendees who trained me and that I hadn’t seen in years, former residents I helped to train, and even colleagues whom I had never actually met in person but who I consulted on cases with at one time or another. I finally got to hug close colleagues whom I have spent texting or calling for months—and even years—of phone calls and texts. I recognized recent and past colleagues all over the room, similar to the Women in Medicine events that initially got me started with TCMS not so long ago. The smiles were genuine and the camaraderie real, making the Travis County community of doctors feel small given how many people I recognized, despite such a large region and growing number of physicians.
I write this account of my late start to TCMS involvement in the hopes that residents and early career physicians don’t wait as long. We need your passion and energy! TCMS is an incredibly welcoming and fun society to be a part of, so I hope you dip your toe in a little and get pulled in just like I did—and soon!
Welcome Home—to TCMS!!!
Blair Walker, MD
tcms@tcms.com
Submitted December 2025
by Dr.Gabriel Millar
The Power to Heal


I have been in private practice in Pediatrics for almost 30 years now. My journey has not always been a smooth sail. The myriads of challenges—both personal and professional—were daunting but not insurmountable.
What helped me get through all of these is my faith in God, my wife and my sons, my parents, my extended family, my dearest friends—and my Art!


Growing up, I thought that one day I was going to be a successful artist, but I knew I did not possess that raw inherent talent. Thus, I settled with the next best thing!
Now, I have the best of both worlds. The work and career that I truly enjoy and the passion in art that I can indulge in without the burden and worry of critiques that artists dread.
I am preparing for my Board re-certification and to help me ease my worry, I read and review and paint in-between in my studio (a.k.a. our spare bedroom). To my surprise and delight, it helps me focus more.
Indeed, art has the power to heal, help me stay grounded, and boosts my self- confidence and self-esteem. I hope that I will be blessed in my retirement years with good health in mind body and spirit to continue painting and—maybe one day—exhibit my art!
Gabriel Millar, MD
tcms@tcms.com
Submitted November 2025
by Dr. Lisa Savage

Keepsakes
Does anyone else have a folder or drawer at the office stuffed full of cards and letters from patients? Maybe these days it’s more likely to be a digital file but keeping a collection of thank you notes or other mementos from grateful patients is an easy way to bolster your confidence or serve as a reminder of the good that you are doing. It can also be a trip down memory lane that spans the arc of your career to remind you of how many patients you’ve taken care of, how far you’ve come as a physician, how many lives you’ve touched.
I had such a folder in the bottom drawer of my desk when I had my brick & mortar practice. When I was moving out of that office, emptying out my desk, I came across that messy, wrinkled and over-stuffed folder and got distracted from the task at hand by its contents. I was touched by how the busy women who were my patients (and a few of their husbands) took the time to write and send or bring me something I could hold in my hand, something I could save. Sometimes the cards contained a picture of their baby or toddler or teenager (!) whom I had delivered. Other times it was just a sweet note of thanks or remembrance. That folder sustained me on those occasional bad days we’ve all experienced when a patient was unhappy or wrote a negative online review. It can be so easy to fixate on one patient’s perspective or unmet expectations and forget about the hundreds of others whose gratitude you earned.
And wow, how the items in that folder grew when I sent out the letter to my patients announcing the closure of my in-person practice. Those alone needed a new folder! I ended up transferring all of it to something sturdier, one of those keepsake boxes you get at the hobby store, that I will continue to treasure and sit down with from time to time.
Two favorites stand out. One letter was from a husband whose wife had a stat C-section for fetal distress. I loved a good stat section, but this one was especially stressful. Afterward, with a good outcome, I went on with my day, week and month as usual. Around the time of the patient’s postpartum appointment, I received her husband’s letter, and in it he said I was brave. Brave! I had never thought of myself as brave, but seeing it through his eyes, I was both flattered and humbled. I know the entire L&D team looked like heroes to him, while we were just doing our job. But bravery is something each and every one of us physicians has, whether it is displayed dramatically or not. It takes courage to enter that exam room, wield that scalpel or sit with someone for whom you have little else to offer but your presence.
The other favorite was a completely unexpected note from a patient who wrote in sympathy and support when she heard about a trying medical practice experience I went through that had nothing to do with her. I keep that one separate, in my desk drawer at home. She has no idea what an impact she made on me, but in the midst of a difficult time in my career, she was kind enough to write. I saved her note as a welcome reminder that even in the midst of trials, there are many patients who sing our praises.
Keep those cards, print out the emails, make a folder; eventually you will need a keepsake box. At the end of a tough or extra busy day at work, take a few minutes with what’s in your collection. Sift through all that affirmation when you wonder if what you are doing is making a difference or feel the weight of balancing all your roles or want an alternative to perseverating about the Yelp review. It’s free and always available. Gratitude from our patients is common, of course, but when it is expressed in writing, you can hang onto it as a tangible reminder of how much you are valued and appreciated.
Lisa Savage, MD
tcms@tcms.com
Submitted November 2025
by Dr. Sheila Shung

Tennis Saved Me
What gets me out of bed every day?
My husband and I have done a pretty good job of raising our two children. They are independent and well-adjusted young adults controlling their own destinies.
The daily household chaos is gone.
My work at my clinic for the past 23 years is routine—no catastrophic events, most of the time. My patients are well-known to me by now.
Life is now quiet and routine…but certainly not mundane.
After 4:30 p.m. on most weekdays (and even earlier on Friday!), I am a free bird. The first thought that comes to my mind when I open my eyes every morning: Who am I playing tennis with today? What? Laura again? The devilish tennis rabbit who runs me all over the court? Well, I better hustle and get ready!
Tennis saved me. It’s been five years since I first picked up a tennis racket, after the tennis courts opened up toward the end of the pandemic. Since then, I have met many women who are in the same boat as me, trying to relieve stress from a day’s work. I never imagined that I would become the captain of multiple tennis teams leading 40 to 60 mostly women players playing U.S. Tennis Association’s league matches every week. These women are my inspiration—most of them still have young children at home, with many more responsibilities than I, but give their best every week on the tennis courts. I have become the team mom. It is now a tennis sisterhood, celebrating life and supporting one another.
On rare days I can’t play tennis due to weather, I fall back on sewing and quilting. You would not believe I could sit for that long if you knew me! Quilting got me through the pandemic. After signing off from virtual patient visits every day, I cut big pieces of fabric into tiny pieces of fabric, then sewed them back into a big piece of quilt—a piece of art. Believe it or not, quilting preserved my sanity.

The quilters have a saying: "When life falls to pieces, make a quilt."
How does one balance the demands of work and life? Advice I give to my patients: do something for yourself every day. Even if it is for 15 minutes, do it! Whatever will make you happy for those 15 minutes, do it! You will be amazed at how much you will look forward to doing something that will make you happy, and how much it will help you get through your daily grind.
Looking at one of my physician friend’s photographs always make me smile. He took pictures of highways, wildflowers, hospitals at dawn, hospitals at sunset and whatever he saw that day. I bet that made him very happy. Sharing the pictures made me feel his joy.
When you wake up in the morning, before all of the chaos, responsibilities, demands, and text messages crush upon you, ask yourself: "what am I going to do for me today?
Sheila Shung, MD
tcms@tcms.com
Submitted November 2025
by Dr.Tony Aventa

Keeping Your Balance
I do not believe myself to be an expert in physician wellness, but as a friend recently told me, "Wellness is not one size fits all."
As we strive towards meeting the challenge of increased work-life balance, not all of us will pursue art, poetry, or photography. During my early career, I enjoyed participating in triathlons, but nowadays playing pickleball with my wife and taking the occasional outdoor vacation have filled that role. Not surprisingly, in our current healthcare system developed on volume-based care, trying to achieve that work-life balance becomes more difficult. I have always worked towards passionately protecting my patient-physician relationships. It is one of the core beliefs that I take into the State Capitol when participating in First Tuesdays. It is hard to say how long the bonds of that relationship have been strained, but I suspect from our end increasing costs, regulations, need to see more patients, non-patient facing work, and the computer screens between me and my patient contribute to that stress.
I recently read an article by Dr. Lara Kunschner Ronan, a retired neurologist/neuro-oncologist, reflecting on her retirement process. She wrote, "Eventually it was time for me to move on, to leave the stress and the toll it was taking on my personal life and my ability to enjoy my job." She also reflected on her range of emotions through the process, including "relief, happiness, relaxation, but also a sense of betrayal, anger, and grief. The strangest emotion has been a persistent feeling of guilt." The passage that really hit home for me was "the physician identity development ingrained during my education and training had burrowed deeply into my psyche and is the little voice on my shoulder that even now continues to say, ‘You are selfish to prioritize yourself’.” Dr. Kunschner Ronan agrees that many patients and colleagues will be supportive of our personal decisions but writes, "many more will judge you for failure to uphold your tacit contract with society, for your lack of loyalty, for your personal failings and lack of resilience."
With many of these emotions swirling in me over the past year, I have investigated solutions to move from a volume-based care model to one that is more patient-centered. I am currently going through a bittersweet transition phase which I think will lead to a more fruitful continuation of my patient–physician relationship. I believe I will be getting back long-lost time to spend with my patients and really drill down to meet their needs. I will admit to you, my physician colleagues, that this pathway brings with it
many challenges for medicine as a whole, but I am unbelievably fortunate to have the support of my physician partners as I continue to practice in this new patient care model.
For me, the time to protect and prioritize my relationships with my patients is now. My hope is that this transition will also allow me the opportunity to more fully appreciate the life side of the work-life balance equation.
Tony Aventa, MD
tcms@tcms.com
Submitted November 2025
by Dr. Nilanjana Dasgupta

The Symphony of Two Lives
The path to becoming a physician is often described as a marathon—a relentless test of endurance and focus. For a woman carving out her career, this journey is often a duet, the demanding melody of medicine intertwined with the powerful rhythm of family life. My own journey as a physician began as a long-held dream, but it truly found its unique harmony when I became a mother during my chief residency. Suddenly, the sterile walls of the hospital shared space with the vibrant, messy reality of home.
The years that followed were a joyous, breathless balancing act. My calendar became a testament to this duality: morning rounds ceded to afternoon soccer games, the gravity of a patient’s diagnosis was replaced by the lighthearted chatter of a parent-teacher meeting, and the precise measurements of pharmacology gave way to the comforting science of cookie baking with a cohort of other physician-moms. It was a life lived at full volume, a constant and beautiful tension between fulfilling my deepest professional ambition and embracing the transformative identity of motherhood.
As I look back now, it wasn't a Herculean effort that kept me from burning out; rather, it was the deliberate cultivation of four foundational pillars that instilled joy, excitement, and a profound sense of wellness to begin each day and look forward to work.
Pillar 1: The Anchor of Mission
Roughly a decade into my career, I experienced a powerful professional recalibration. I realized my deepest satisfaction was not a matter of prestige or pace, but mission. This connected me back to my medical school days—I trained at Mahatma Gandhi’s rural institution where prevention and community health were the key focus. Specifically, working within an FQHC (Federally Qualified Health Center) model focused on the senior population now gives me the most pleasure. This work is holistic, rooted in community, and fundamentally focused on dignity. Aligning my daily practice with a mission that speaks directly to my values provides an enduring sense of purpose that transcends the administrative burdens and emotional fatigue of healthcare.
Pillar 2: The Lifeline of Community
The second, and perhaps most vital, pillar is my "besties": a group of physician moms. This community is forged in the trenches of simultaneous professional and domestic urgency. They are the sounding board for an impossible patient case and the emergency contact when school pick-up clashes with a critical procedure. We lean on each other to vent, celebrate, and normalize the inherent chaos of our lives. This non-judgmental, mutual support system is a powerful buffer against isolation, acting as a crucial decompression chamber.
Pillar 3: The Dedicated Identity of a Mom
I learned that true balance isn't about perfectly merging two identities but about dedicating time and space to each one independently. I had to consciously commit to building an identity as a mother and a wife separate from my identity as a physician.
Leaning and connecting with other families while building a “circle” of friends who have become like family is invaluable. This has created a consistent deep-rooted sense of love and belonging for my children and me that we always carry with us.
When I am at social gatherings, celebrating a festival, or helping with a school project, my white coat is metaphorically left at the door. This mental boundary-setting allows me to be fully present in both roles, ensuring that I am recharged by the small, sacred moments of family life.
Pillar 4: The Freedom of Unburdened Time
Finally, I discovered the profound importance of carving out space to be simply me. For me, this sanctuary manifests in two hours a week of Bollywood dance. For those 120 minutes, I am neither a physician nor a mother. The weighty responsibilities of my primary roles dissolve. I am simply following rules and instructions related to steps, enjoying the music and the rhythm. This deliberate act of engaging in a non-essential, purely joyful activity is a vital cognitive reset. It is a moment where my mind is fully occupied with a task that has no life-or-death consequence, allowing me to return to my professional and maternal duties with renewed energy and perspective.
Wellness for the physician-mom is not a singular achievement, but a continuous act of intentional orchestration. It is the commitment to a mission that gives work meaning, the cultivation of a community that provides emotional ballast, the protection of family time that grounds the self, and the pursuit of unburdened joy that fuels the soul. It is this finely tuned symphony of responsibilities and retreats that ensures I greet each new day—and each new patient—with excitement, compassion, and resilience.
Nilanjana Dasgupta, MD
tcms@tcms.com
Submitted October 2025
by Dr. Esther Yaniv

Inviting Forgiveness
Every Saturday morning, I forgo the luxury of sleeping in—something I feel I’ve rightfully earned after a long week. Instead, I find myself springing out of bed, energized by anticipation. While the streets remain quiet and free of traffic, I willingly make my way downtown to the yoga studio where I teach.
Teaching yoga became a gift I offered myself, without any idea of where it might lead or the lessons it would bring. After practicing yoga for several years, I was encouraged to join the teacher training program, primarily as a way to deepen my own experience. I had no initial intention of teaching.
In the early years of guiding classes, I was often critical of myself whenever I made mistakes. Missing a pose in the sequence or mixing up left and right would completely unsettle me. In those moments, I felt like a failure—ashamed and inadequate—yet each misstep became an essential part of my growth as a teacher. What I hadn't realized was that I was also evolving as a physician. The insights and challenges I encountered as a yoga instructor began to influence and strengthen my abilities in the medical field.
As a physician, vigilance against errors is paramount—mistakes can have serious, sometimes dire, consequences. The principle of "do no harm" perpetually underlies every medical decision, fueling questions like, “What if I miss something?” or “What if my diagnosis is wrong?” Over time, I recognized that this mindset had subtly permeated my approach to teaching yoga.
By drawing this connection, I began to see that mistakes need not be sources of relentless self-criticism. Instead, they can become opportunities to practice creativity, flexibility, and kindness. Mistakes invite forgiveness, humility, courage, honesty, and resilience. These qualities, cultivated on the mat, began to influence how I viewed both myself and my professional practice.
In a profession constantly challenged by bureaucracy and never-ending demands for efficiency, self-compassion becomes essential. While it is healthy to question and doubt—it keeps us sharp—there is little benefit in being relentlessly hard on ourselves in every facet of our work. What if we embraced humility not as a weakness, but as a strength in medicine?
My belief is that if we allowed ourselves this grace, we might find ourselves—like I do on Saturday mornings—leaping out of bed, ready and eager for the day ahead.
Esther Yaniv, MD
tcms@tcms.com
Submitted October 2025
by Dr. Rebecca Kim

The Doctor as Artist
I have gone through different phases—figurative drawing, botanical illustration, animal paintings. There was a time that I did portraits of my pets, because they are such good friends and make me feel better no matter my worries or anxieties.
They each have unique personalities and their own little quirks. After one of my dogs died, I was glad that I had small remembrances of him later—even though it was poignant and bittersweet.

The little white dog is Sherman—he was full of charisma and personality. One dog trainer told me he was in my life to teach me not to be a doormat. He had a tan heart-shaped patch on his back.

The cat is Madeleine Grace, and I believe she is cat royalty.

The little chihuahua mix is Clementine. She is the opposite of Sherman - a bundle of nerves and anxiety and very vocal. She's a little chihuahua and needs to express herself!
There was also a time when I took a sabbatical several years ago to a tiny little city in California. I needed some respite and solitude after burnout, which can happen at different times in our lives. I rediscovered drawing to combat stress, doing some pen and ink drawings while wandering around. I met a writer there who encouraged me to find little vignettes and just start drawing.
Rebecca Kim, MD
tcms@tcms.com
Submitted October 2025
by Dr.Brian Sayers

The Evening Star
On those rare evenings when I am sitting, undistracted, by a fire next to a pond at our weekend getaway in Fayette County, I become an amateur astronomer. Living in Austin, we see very little of the magnificence of stars on a clear night. Much like my identification of bird species on the property, I mostly fabricate the names of constellations and those around me either don’t mind or just ignore my babbling—but some things in the sky are unmistakable.
I’ve been considering the Evening Star recently, partly because of people we have lost in our medical community these last few months. Far brighter than other celestial bodies, the Evening Star shines low on the western horizon at dusk, just as, later, the Morning Star does on the eastern horizon with the approach of dawn. It is the visible manifestation of the orbital cycle that Venus travels: it shines as the Evening Star for 263 days before disappearing for 50 days, then reemerging as the Morning Star for 263 days before disappearing again.
Years ago, in another lifetime, I was an internal medicine resident in Albuquerque. New Mexico in general, and our patient population at County and the VA in particular, was a blend of direct descendants of the Spanish and the rich Native American heritage of the Navajo, Apache and other tribal cultures. In the mid-80’s when hospice care was in its infancy, it was not uncommon for patients to be hospitalized for terminal care at the VA. Alberto is one who I vividly remember. He had strong Mescalero roots and one evening his daughter recalled ancient legends about death, something I still think of when someone I care about dies. It involves the Evening Star and its endless cycles of darkness into light. According to some legends, the Evening Star is a celestial conduit, a spiritual guidepost that gently guides the deceased into the spiritual world, their eternal spirit eventually reemerging as the bright star in the east that heralds a new day. It is a legend that gives hope to the dying and those they leave behind.
We are a large medical community in Austin and most of you may be unaware that we have lost several of our colleagues these last few months, colleagues in the prime of their lives and medical careers, each death bringing with it shock and grief within their smaller communities. In church this morning our minister spoke of grief as a kind of exile, our return often accomplished with time and the help of community. Integral in the concept of community is a sense of belonging, a sense of shared concern, a sense of support. Our medical society has shown itself to be a caring, loving community. We accomplish many things—advocacy, community leadership, and support of local programs. But increasingly important, we are also called to support and care for each other in the many ways it is needed, and when it is needed most. The face of how that support is offered must adapt with the changing needs of our colleagues and circumstances of our profession, but the need for us to reach out, individually and collectively, is always there.
When I am sitting admiring the evening sky, I look for the Evening Star first, as it will disappear not long after dark. Finding something predictable is reassuring when so much around us is so unpredictable. My faith reassures me about death, and beyond, and that gives me comfort, but I also love Native American lore about the spiritual pathway of the Evening Star, of the hope and reassurance that the Morning Star is not far behind.
Brian Sayers, MD
Chair, Physician Health and Rehabilitation Committee
tcms@tcms.com
Submitted September 2025
by Dr. Holli Sadler

Networks of Kindness
For as long as I’ve been practicing medicine in Austin, I’ve had the privilege of working closely with local internal medicine residents. Residency is an intense and demanding time, but it’s also a period of profound growth and transformation. Watching the process unfold over three years—seeing a hesitant intern grow into a confident physician—has been one of the great joys of my professional life.
Because of my involvement in GME, my clinical practice has often taken non-traditional forms—shaped by community needs, time-limited opportunities, and very, very, limited budgets.
One of the most meaningful projects I’ve been a part of emerged several years ago, thanks to Dr. Lysbeth Miller, then-director of the residency program. She wanted graduating residents to experience home visits—not as medical providers, but as learners. We decided each resident would choose a patient they’d got to know well during training—either someone from their clinic panel or from frequent or prolonged hospitalizations—and, with the patient’s consent, visit them at home. The goal was to shift the lens: to interview patients not about medications or symptoms, but about their lives. We framed it with language about identifying social determinants of health and environmental barriers. But, at its heart, the project was about connection. It gave residents permission to slow down, to listen, and to reflect. And in doing so, it reminded all of us why we chose this profession.
The visits often surprised us. They revealed the extraordinary and quiet ways people survive and support one another. I remember homes that weren’t traditional houses at all—spaces patched together through networks of kindness. One patient lived in a converted shed, kept warm by a neighbor’s extension cord. Across town, a church group checked on a man every morning and if he was not in his expected location, they knew to call the hospital, then the jail—in that order. We went to houses where full families shared a single bedroom and the kitchen was a shared space, functioning like a cooperative.
These were not programs or policies. Rather, they were acts of trust and human kindness.
Over time, I came to think of those home visits as more than an educational tool. They sustained me. They filled my cup. I never left a visit without feeling a little more hopeful about the world. I learned about my peers—physicians in our community who quietly delivered high-quality, compassionate care to patients others might have overlooked.
Though the formal project has ended—the timing no longer quite right—I carry those experiences with me. They remind me that medicine is rooted in relationships. Even now, I can find moments to practice “slow medicine”—to pause, to witness, to honor the humanity.
We all have our own anchors in this work—those people, places, or rituals that remind us why we started and why we stay—patched together through our own networks of kindness.
Holli Sadler, MD
tcms@tcms.com
Submitted September 2025
by Dr. Rchard DeBehnke

Hidden Heroes
Special moments often arrive unexpectedly and leave lasting impressions.
In my training as a resident on the hospital endocrine service, I was hastily checking on patients before morning rounds. The nurse alerted me that the lab for "Mrs. Y" was abnormal. I quickly reviewed it, glanced at her medical regimen, and hurriedly adjusted her medication…incorrectly. I moved on to check the other patients on the service, but before I could leave to start rounds with the attending physician, the nurse urgently called about Mrs. Y’s bedside glucose readings. I rushed back, saw what I had done, and made the necessary adjustments. Now late for rounds, the nurse who noticed the abnormal glucose readings informed me that the attending physician was in the break room and would like to see me.
My heart sank. My mistakes had been revealed. I was to be made a public example to hammer home a teaching point, something we all have experienced in our medical education—our own version of the public stocks.
I entered the breakroom and found the attending, "Dr. R," sitting alone.
“So, what happened with Mrs. Y this morning?” he asked. I told him that I had rushed through things, that I hadn’t taken the time the patient needed, and that I was mortified by what I’d done.
Dr. R stood up, straightened his jacket, looked at me, and said, “What can I say, Chief, you screwed up. Let’s go make rounds.” And with that, he walked out onto the ward. Stunned by the brevity of his confrontation, his familiarity, and his vulgarity, I quickly followed.
In an instant, Dr. R delivered a series of lessons:
He was disappointed but believed I was a better doctor than I had shown that morning, and he expected me to be that doctor moving on.
Owning your mistakes is the path to learning from them.
He had the grace and patience to know he was teaching humans and the idea of how to motivate them.
Sometimes what is left unsaid is more complete and powerful than what is said.
Richard DeBehnke, MD
tcms@tcms.com
Submitted September 2025
by Dr. Vani Vallabhaneni

Yoga for One Earth, One Health
June 21st was the longest day of the year in the Northern Hemisphere. It was also “The International Day of Yoga,” recognized by the UN General Assembly in 2014, since yoga has significant health benefits. A total of 177 nations co-sponsored the resolution, which is the highest ever for any UNGA resolution, and was adopted unanimously.
Yoga originated in ancient India more than 5,000 years ago. The word “yoga” comes from Sanskrit root “yuj” meaning “to unite"—referring to union of body with mind, individual self with universal consciousness and breath with movement. When this union happens, we are able to connect more easily with our awareness, our inner self. We are able to use our intellect rather than relying on instincts. We can be more thoughtful and rational, responding instead of reacting.
Yoga practice is more than just stretching or exercise. It includes:
Physical postures (asanas) that help with stretching and strengthening the muscles and improving flexibility, range of motion, balance and posture.
Breathing techniques (pranayama) that help regulate our breath, improve lung capacity, calm the nervous system, and boost energy and focus.
Meditation & Mindfulness which help us take an inner journey and to be more self- aware. Meditation lowers cortisol level, increases endorphins, and reduces overall inflammation in the body. It trains the mind to be in the present moment, reduces stress and anxiety, and cultivates inner peace.
Ethical principles and Lifestyle (yamas & niyamas) which give guidelines for how to treat others and yourself with a foundation in values such as honesty, non-violence, self-discipline, and contentment.
With stress, anxiety, depression, and insomnia on the rise in modern society, it is more important than ever to practice yoga regularly and help our family and patients do the same. Deep breathing, yoga stretches, and meditation can decrease our stress response through reducing cortisol, and decreasing chronic stress can reduce burnout.
Anyone can stretch and deep breath comfortably in his/her own home as well as at work! It can be as simple as sitting back, closing your eyes, and taking a couple of deep breaths for one minute.
I routinely guide patients in my sleep medicine practice to explore yoga techniques by taking classes in their community or at their gym to improve their sleep. Meditation may be an effective behavioral intervention in the treatment of insomnia and can improve emotional well-being and mental health.
It is also a good practice to include a few minutes of yoga stretches, meditation, or deep breathing techniques at work before a meeting or before the start of the day. It can improve teamwork and decision making for the greater good of the organization. When leaders start their day with a practice of yoga and meditation, they can make better and more thoughtful decisions, and the organizations can thrive and be more successful.
My own practice of yoga started very early, as my school in India had yoga incorporated into PE class. I learned meditation and pranayama more recently and practice regularly. My favorite part of yoga is sun salutations. I find it very challenging to do some yoga asana and am still trying to master the sequence of moon salutations. I incorporate yoga into my life by joining group practice with my friends every Sunday morning and by being part of an online yoga community.
As you start your practice, go slowly and listen to your body. Use your breath to guide you into a yoga stretch. Learn under the guidance of an experienced and certified yoga instructor. Certain medical conditions such as heart disease or arthritis may require modification of your own program.
Yoga can be part of every physician’s wellness plan.
Vani Vallabhaneni, MD
tcms@tcms.com
Submitted August 2025
by Dr. Jerry Fain

The Gift of Empathy
As a practicing hematologist/medical oncologist in Austin since 1996, I had seen firsthand how patients’ lives were changed in an instant from the diagnosis of a potentially life-threatening disease. However, it wasn’t until I was the patient that the full appreciation of the magnitude of such an illness became apparent. Although I was empathetic to the patients’ feelings, concerns and frustration, it never occurred to me that being a patient could change my practice as a physician. What transpired next was as life changing as the illness itself.
What started as a beautiful bike ride on a family multisport vacation in Jackson Hole, Wyoming early in the morning of July 21, 2014, would soon change in an instant. At the end of the ride there was an abrupt onset of sharp, stabbing, intermittent thoracic back pain with paresthesia in the back. I was having an acute anteroseptal MI. Fortunately, the decision was made to give TPA in the 2 bed ER in Jackson Hole and not wait to be transported by helicopter to the closest cardiac facility, a decision that no doubt saved my life. After a 4-day hospital stay, we returned to Austin and all was well until the morning of July 27, 2014, at 7 am when I experienced a v-fib arrest at home. Having a fire station 1 block away proved to be another blessing as the firemen were at our house within 2 minutes of the call. Having a physician spouse and an 18-year-old daughter who had just received BCLS certification at Westlake High School was another blessing. Five days later, after a defibrillator/pacemaker was placed, I returned home.
Upon returning to clinical practice, one of my long-term patients requested an appointment at the end of the workday. She wanted to be my last patient of the day, and it came as no surprise that she asked me to describe to her what had transpired during my 6-month absence from work. I had taken short term disability to recover. It soon became apparent that this appointment was not about her but about me. As a senior research scientist in Psychology at UT Austin, this patient had practiced clinical psychology for many years. She asked the open-ended question “and how are you doing now?” Without thinking, I described my inability to sleep since my discharge from the hospital August 1, 2014, due to pulsations in my ears and a bounding pulse. To me this was the physiological result from a reduced Ejection Fraction of 35%, and a previous MI; however, to a trained PhD in Psychology these were symptoms of anxiety, PTSD and possibly panic attacks. With her guidance I learned how to relax through deep breathing and guided meditation and, to my surprise, the pounding in my ears stopped.
Although the medical treatment had saved my life, it was the mental component of my illness that took me by surprise. Having validation that my symptoms were self-induced but treatable was very powerful and reassuring. So, from that day forward, whether it be a long-term patient or a new patient encounter, I took the time to ask my patients how they were coping with their illness. It became readily apparent that many of these patients with cancer were suffering from some form of PTSD and almost daily anxiety. I finally understood just how devastating cancer, or any potentially life-threating illness, could be. Patient after patient told me that the best thing that ever happened to me was having a heart attack, because I understood their angst, their fears and their thoughts because I had faced death and lived day to day with the 30%/year chance that I might suffer another cardiac arrest.
Now, some 11 years since that event, I still appreciate and recognize the psychological ramifications that illness of any kind can bring to a patient. Learning, it seems, can occur in any circumstance, and the events of July 21 and July 27 changed my life, my medical practice and every aspect of daily living. Although the panic attacks have resolved, the deep, dark memories and fears surface with each vacation, but with deep breathing and relaxation techniques provided by this special patient, I have lived another 11 years with some normalcy. My path to wellness included the skill of my doctors as well as an unexpected and timely gift from a very special patient.
Jerry Fain, MD
tcms@tcms.com
Submitted August 2025
by Dr. Belda Zamora

Dr. Zamora and her father, Dr. Santiago Zamora
Finding Joy in Medicine
In our weekly physician wellness emails, one truth consistently shines through: each of us carries stories—moments and memories—that define who we are in this sacred calling.
I’ve been a family physician for over 25 years, a journey I began alongside my late father, Dr. Santiago Zamora. Today, I continue that path with my uncle, Dr. Pete Zamora, carrying forward a legacy rooted in service, compassion, and community.
There is a deep joy I find in caring for my patients and, often, their entire extended families. Over the years, these relationships evolve—we become witnesses to the births, illnesses, recoveries, and losses that shape their lives and ours. But with that honor comes weight. The privilege of walking with families through joy also means standing with them in grief. And when they suffer, we feel it too.
So how do I continue to find joy in medicine?
Most days, you’ll find me out on the trails—hiking, biking, or running in the Austin outdoors. Movement in nature offers me sacred space to reflect, grieve, and decompress. On lunch breaks, I often walk around Town Lake. Sometimes I go there to quietly mourn a patient I’ve lost, to process what I couldn’t in an exam room.
My greatest test came during the years I cared for my father—himself a pillar of family medicine in East Austin for more than four decades—as he navigated the painful decline of dementia. At the same time, my oldest son left for college out of state. I had to learn how to stop being the doctor and simply be a daughter. My days were a blur—rushing through patient appointments, squeezing in lunches with my father, and returning to the clinic, before ending my evenings with my two younger children at home. My weekends, too, disappeared into caregiving.
And yet, even then, joy would find a way in.
I was lucky to have a circle of strong, supportive women at my spin studio—our 5:30 a.m. crew. During this time, Belinda Clare (TCMS CEO) must’ve seen the fatigue in my face. She often encouraged me to reach out to the Physician Wellness Program (PWP) - but like so many of us, I kept saying I didn’t have the time. Still, their presence, their encouragement, their simple acknowledgment of the load I carried—that mattered. It reminded me I wasn’t alone.
Today, I still find joy in medicine. Despite the long hours, the emotional toll, the quiet heartbreaks—it’s still there. I believe the key to sustaining that joy lies in tending to ourselves, just as we tend to others. It’s in making space for grief, in choosing movement, in leaning into our communities—both professional and personal.
To those walking this road beside me: you are not alone. Your joy is not frivolous. It is necessary. And it is worth protecting.
Belda Zamora, MD
tcms@tcms.com
Submitted August 2025
by Dr. Robert Duhaney

Me with the family at Niagara Falls, Ontario, Canada - June 2025
Learning to Live Life Fully
A Physician's Story of Family, Faith, and Renewal
As a primary care physician and office medical director, I often find myself pulled in multiple directions—between patient care, administrative responsibilities, and the ever-evolving demands of modern medicine. But alongside this professional identity, I am a husband to my wonderful wife, Kelli, and a father to three vibrant teenagers. Learning to balance these two worlds—medicine and family—has been both my greatest challenge and greatest gift.
After completing my residency in internal medicine in Maryland in 2008, my wife and I relocated to Dallas, Texas, for my first position at a busy internal medicine clinic. I joined two experienced physicians who modeled deep dedication to their patients. Their work ethic was admirable, but over time, I noticed how often that commitment came at a personal cost. They seemed constantly stressed, and the strain of long hours and unrelenting patient care seeped into even the quiet moments of the day.
It didn’t take long for me to fall into that same rhythm—long clinic days, charting after dinner, answering messages late into the night. I told myself this was what it meant to be excellent. After we had our 3 kids and I continued trying out different practice set-ups over the past 12 years, I began to feel the toll—on my body, my spirit, and most of all, on my family. My children were growing up quickly, and I feared missing the moments that mattered. Though my marriage remained strong, it needed intentional time and shared joy to truly thrive. Something had to shift.
That shift started slowly but deliberately. Then the COVID-19 pandemic disrupted everything. Like many families, we found ourselves re-evaluating our lives. My wife and I looked at each other and asked, Is this our moment to reset? The answer was yes. I applied to a national primary care group—One Medical—that was opening a new location in Austin. After several interviews and much reflection, I accepted the offer, and we made the move in 2021.
Relocating gave us a fresh start. I began viewing this new chapter as a chance to double down on what mattered most: time with family, cultivating new friendships, and rediscovering joy outside of medicine. We made it a point to prioritize family dinners, show up at school events, and create simple weekend traditions like Saturday morning breakfast together.
I also rekindled one of my favorite pastimes: tennis. These days, my wife and I play regularly—sometimes attending clinics, other times just rallying for fun at an available court. It’s not just exercise. It’s laughter. It’s connection. We’ve even built friendships through tennis, meeting other couples for casual matches and post-game chats. These moments on the court have helped strengthen our marriage and brought a sense of play back into our busy lives.
Equally important has been staying rooted in our faith community. Our church has become more than a place of worship—it’s a place of belonging. Whether we’re facilitating small group gatherings, volunteering as a family, or enjoying meals with fellow church couples, these gatherings offer a spiritual reset and emotional grounding. They remind me why I chose internal medicine in the first place—to build long-term relationships, offer support in life’s toughest moments, and reflect compassion in action.
Saying “yes” to what fills me up—whether it’s quality time with Kelli, cheering on my kids at their activities, connecting with friends, participating in church events, or playing tennis—has helped me show up more fully for my patients and colleagues. I’ve learned that living with purpose doesn’t mean splitting myself into separate parts but integrating the roles I cherish most.
Finding balance doesn’t mean achieving perfect harmony every day. There are still weeks when inboxes overflow, the clinic is busy, and the pressures of leadership stretch thin. But I’ve come to believe that intentionality beats perfection. Each choice I make to align my time with my values brings me closer to the kind of wholeness I aspire to live out.
To my fellow physicians, I offer this encouragement: you don’t have to choose between a fulfilling career and a rich personal life. But you do have to be deliberate. Set boundaries. Protect your rest. Rediscover your passions. Lean into your community. These choices won’t just make you a better doctor—they’ll help you become a healthier, more joyful human being.
Medicine is a sacred calling, but so are marriage, parenting, friendship, and faith. When we give space to nurture all these callings together, we find not only balance—but true purpose and joy.
Robert Duhany, MD
tcms@tcms.com
Submitted July 2025
by Holli Sadler, MD

Ode to That Best Friend from Medical School
Take a moment and conjure up a memory of your best friend from medical school. Maybe you're in the thick of it now. Maybe, like me, it’s been so long you’ve stopped counting. Wherever you are in your journey, bring that person to the forefront of your mind. When did you meet them? What brought you together? When was the last time you had the chance to say hello? How big is your smile when they come to mind?
Her name is Tiffany. She’s from Tomball, Texas, and she remains one of my most treasured friends to this day—all thanks to the quiet foresight of a kind ophthalmologist named Dr. Spiegelman. Dr. Spiegelman taught the eye exam during our first semester. He had a calm, thoughtful presence and an unusual talent for seeing beyond the surface. One day, he pulled me aside and asked, “Holli, have you met Tiffany yet?” I responded that I had not. “She’s in another section of my class,” he said, “and I think you two would really get along.”
It was such a small moment, but I’ve never forgotten it. Dr. Spiegelman had a gentle, unhurried way about him. He noticed things—how people carried themselves, who looked like they needed a connection, who might be quietly drifting in a sea of over 200 classmates. In a place that could feel anonymous, his attention was rare. And it mattered.
I am, by nature, an introvert—a creature of habit who sits in the same spot, keeps to myself, leaves the minute the meeting has ended, and doesn't mind long stretches alone. I didn’t go out much in med school. I studied during the week so I could spend weekends with my husband. Tiffany and I didn’t share a lab group, an anatomy tank, or a clinical rotation. Our paths never directly crossed. Without Dr. Spiegelman’s nudge, it’s entirely possible we never would’ve met. But because he suggested it, I sought her out. I think I said something like, “Hi, I’m Holli. Dr. Spiegelman said we’d get along, so... let me know if you want to eat lunch together?"
That was it. Tiffany has been one of my dearest friends ever since.
It’s rare to meet someone who sees both your strengths and your chaos—who can make you laugh when you're unraveling and remind you of who you are when you’ve forgotten. That’s Tiffany for me. Any time I have a question that touches her specialty, I treat it as an excuse to call. When life gets hard—personally or professionally—she’s often the first person I reach out to. She’s spent long stretches on my couch. I went to Paris to be in her wedding. Her family feels like an extension of mine. She’s been there: for weddings, births, funerals—the full spectrum of life. She understands the pressure, the exhaustion, the desire to do good work and still have something left for yourself and your family at the end of the day.
After one especially demoralizing exam in med school, she called to check on me. I told her, “I feel like a delivery truck ran me over—then reversed for good measure. Let’s just say I’m humbled.” Thirty minutes later, there was a knock at my door. Tiff stood there holding a six-pack of Heineken and a bag of peanut M&Ms. That image of her—kindness in hand, mischief in her eyes—is etched in my memory forever.
In a profession that can be isolating and exhausting, friendships like that are rare and precious. I’m grateful every day that someone took the time to help me find mine.
Dr. Holli Sadler
tcms@tcms.com
Submitted July 2025
by Richard DeBehnke, MD

Regret
Regret is one of those words that carries a very negative connotation. The implication is that regret is a failing, a weakness that we should hide from others, and we should sail through life doing it “our way”. Reportedly, Frank Sinatra disliked his signature song, feeling it self-serving and insincere. In his book “The Power of Regret, How Looking Backward Moves Us Forward”, Daniel Pink agrees and proposes that a better understanding of the workings of regret will help us to make smarter decisions and bring greater meaning to our lives. Also, perhaps, make us healthier. His writing is entertaining, insightful and highly recommended.
In medicine, we are guaranteed to second guess ourselves on a daily basis. An ambivalent response to the regret of a less-than-ideal outcome can erode our self-confidence and our wellbeing. What struck me as I worked through Pink’s book were two things. First, understanding the nature of regret and its benefits could reduce the pressure that we put on ourselves and increase our joy of practicing medicine. Secondly, we rarely discuss regrets with patients during our history taking and doing so could provide additional avenues of therapy.
Whether a regret develops in an active (an argument with a spouse, lying) or passive (passing on a chance to take a new position, opportunities missed) way, it usually takes the form of “if only” or “what if”. Pink categorizes regret into moral failings, insufficient and excessive boldness (overwhelmingly the former), foundational decisions of picking short term pleasure over long term benefits, or loss of connections with friends and family due to rifts or just drifting apart. These categories provide a framework for us to examine ourselves and those we care for.
We all deal with our regrets in different ways. Far too often regrets are ignored or denied. This robs us of a chance to learn from our experiences and too often be consumed by the negative feelings regret generates. However, if we address regret, we can make better decisions, improve our performance by better deliberation, and find insight into ourselves and those around us. We can be catalyzed, not paralyzed.
This is where we as caregivers can find a dual purpose. Pink suggests ways of dealing with regret based on his own personal project, “The World Regret Survey”, a detailed questionnaire survey of over 26,000 people from around the world.
To summarize:
Undo it. “The best time to plant a tree was twenty years ago; the second-best time is tomorrow”. If possible, taking action now can help. If a door is truly closed, then be ready for the next one. If it is still open, then act now.
“At least” it. Find a silver lining. Interviewing medal winners at track meets and the Olympics, findings suggest that the bronze medalists were happier with their result than the silver medalists, by a lot. “At least” I got on the podium, versus “If only” I had trained harder.
Self-disclosure. Exploring one’s regrets is therapeutic. We are often inhibited by a reticence to “bother” someone, but humans are terrible about divining how others will react to their entreaties, overestimating their intrusiveness and underestimating the positive effects of any interaction. Engaging the involved party, journaling or talking with a caregiver can be rewarding.
Self-compassion. Ask them, “If your best friend had experienced or done what you had, what would you tell them?” Have them put distance in their perspective, “what would 2030 you, tell your 2025 version?”
Issues with regret are pervasive and can have health consequences, but we are well positioned to help ourselves and our patients. Thinking and asking about their regrets may be another channel in getting our patients to share what is affecting them and lead to alternative ways of therapy. Encouraging discussions of their regrets will build trust and provide a safe harbor for the discussion of feelings. “When feeling is for thinking and thinking is for doing, regret is for making ourselves better”. We would hope to provide them with the tools and perspective for making themselves better and avoiding being crushed by the weight of regret.
Dr. Richard DeBehnke
debehnker@gmail.com
Submitted June 2025
by Tina Philip, DO

The Road Ahead
It is hard to believe that we have reached the halfway point of the year. As you are all aware, there have been many changes within the Physician Wellness Program (PWP). Since I last wrote to you, a dedicated task force made up of our physician colleagues set out to find the best way to move the PWP forward after the retirement of Dr. Brian Sayers as PWP Chair. The end result was the appointment of a new Steering Committee to provide insight, direction, and inspiration and the creation of a TCMS staff position dedicated to supporting the program. I would like to give thanks to task force members Drs. Richard DeBehnke, Lisa Savage, Louis Robinette, and Maria Monge for the time that they spent thoughtfully working together to create this plan and our TCMS Foundation board for their approval to move forward.
The Steering Committee met for the first time this past Wednesday and it was a productive evening understanding the origin and many facets of the program. The committee will be responsible for overseeing the Safe Harbor Counseling Program, weekly physician wellness blog, continuing medical education, and future program development. It was wonderful to see how the wealth of experience in this group, coupled with a strong commitment to physician well-being, will undoubtedly move the program into the future. I would like to thank Drs. Richard DeBehnke and Sujata Jere for stepping up to lead this committee as chair and vice-chair.
To provide support to the Steering Committee and ensure that the program has the resources needed, Michael Warburton was brought on earlier this month as Physician Wellness Program Manager. Michael previously worked with TCMS affiliate organization, We Are Blood, as the Volunteer and Grants Manager. With a bachelor’s degree in communications and a Master of Arts degree in Counseling, he has worked within the Austin nonprofit arena for over 25 years. He has already hit the ground running and brought so much valuable insight and creativity, and we are so glad to have him with us.
Although there have been many recent changes, the mission of the Physician Wellness Program remains the same: to support physician well-being and foster a culture where physicians feel valued, supported, and empowered to maintain their own health and balance while delivering exceptional care. This program is for our physician family and we can all play a role in making it a success. We love to hear the many voices of our community, so please contribute to the program by sharing a creative piece for our weekly blog and encouraging your colleagues to do so as well. The Physician Wellness Program also relies on the generosity of our donors, so consider making a monetary donation at the link below. Thank you to our physician members for your continued support. I look forward to seeing all that we can accomplish together.
PWP Steering Committee:
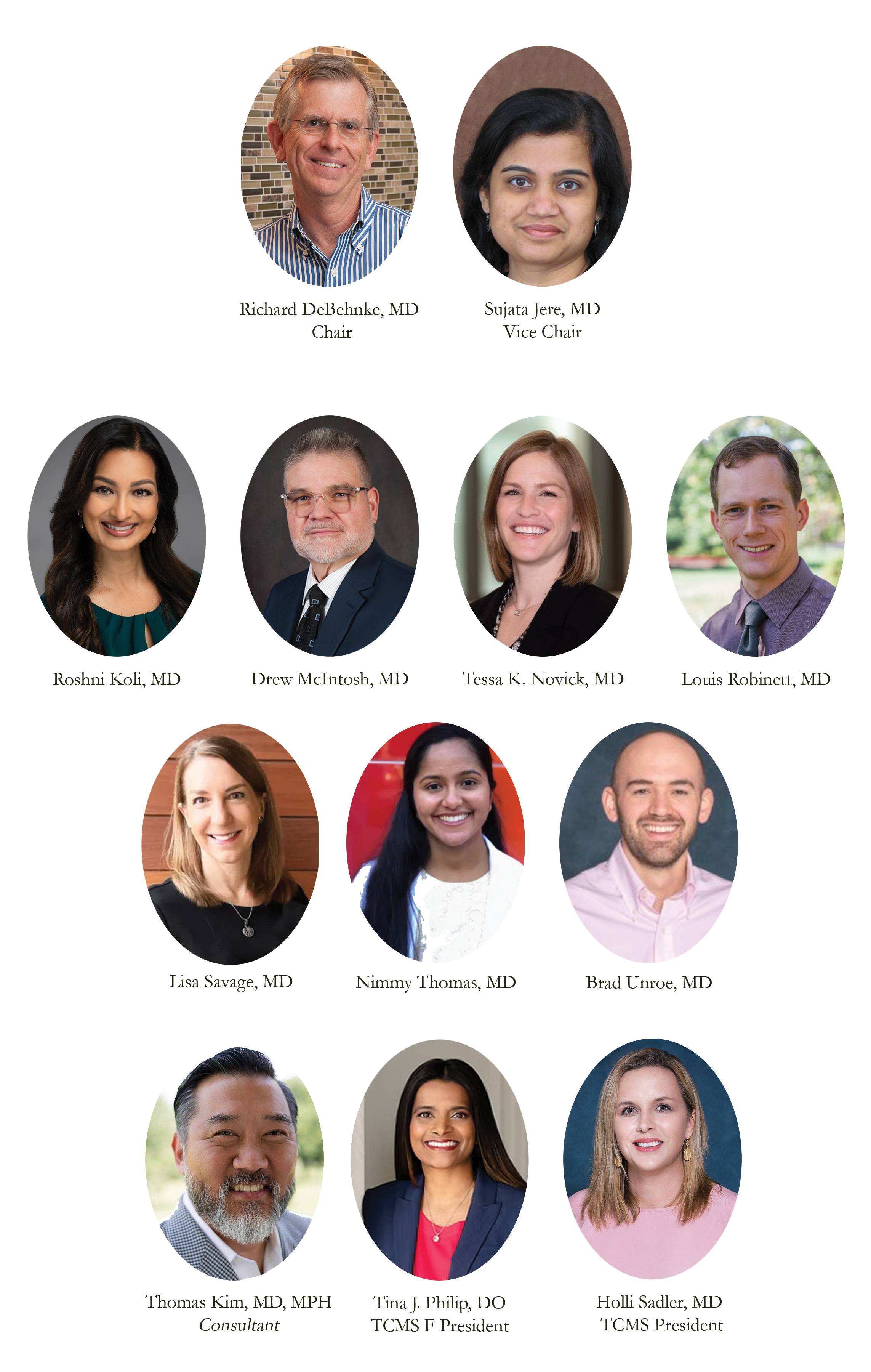
Dr. Tina Philip
tina.philip@gmail.com
Submitted June 2025
by Bob Emmick, MD

Carpe Diem
Everyone knows what free advice is worth these days, but I will attempt to offer something valuable in 600 words or less. First though, I must admit that we are privileged to practice the best profession in the world, in my opinion, and if someone has reached the point that they absolutely dread getting out of bed and going in to see their patients, I would seriously recommend professional help, changing professions, or retiring. People can debate whether we should feel joy in our profession, but satisfaction in listening to and helping our patients I believe is attainable every day.
Here is my advice. It is useful to have goals, but we should experience life to its fullest both in our profession and when we are at leisure, recharging our batteries. I will focus on the leisure side of life when we are seeking peace and joy, that period of recharging, but the thought process can be applied to our professional lives as well. I do not believe in the concept of bucket lists, nor the use of rankings that one thing is better than all others. Instead, I believe that life is to be experienced to its fullest and that each experience can be appreciated for what it offers.
As I understand it, the concept of the “bucket list” is to experience something once then check it off before moving onto the next experience on said list. There is a basic flaw in this, in that no two experiences of the same thing are alike. As an example, I would suggest the eruption of “Old Faithful” in Yellowstone. You cannot compare watching Old Faithful at sunset, in the middle of winter with snow covering the base, or late at night with stars and the moon in the background when no one else is around. A second example slightly to the south of Old Faithful is sunrise at Oxbow Bend in the Grand Tetons. Is it best seen in the spring when you may have a bear or moose swimming across the Snake River, or in the fall when the leaves have changed their color? I dislike the “one and done” approach because you have deprived yourself of the other opportunities. Seek out the experience and appreciate what it offers, multiple times if possible.
Focus on appreciating the experiences and not trying to rank them in order of the best and those that follow behind. During my first year of medical school a group of us went to Cozumel on Christmas break. There we went to dinner at Carlos and Charlies. On the wall was a set of “Rules.” I do not remember the others, but I will not forget the first. It said,”1. You are on vacation so eat something that you do not eat at home.” That has stuck with me, and I have expanded it into the concept of not ranking experiences but trying to savor as many as possible. Should you try to rank the best meal or trip or sunrise or sunset that you have experienced? Can they be ranked, and if so, why? I suggest that we should seek out the experience and enjoy it for what it is. Then savor the memory that will recharge your batteries in the future, not whether it was a check on your “bucket list” or number 1.
I hope that this perspective has helped someone other than myself. In the end it can be summed up in just two words, Carpe Diem!
Dr. Bob Emmick
remmick1963@yahoo.com
Submitted June 2025
by Louis Robinett, MD

Sunsets and Sonship
In April of this year, my wife, 15-month-old son, and I took a trip to the East Coast for a long weekend to visit friends. This was my son’s first flight in a while, and I recognized that this might be a special moment for us. He held my finger while we walked around the terminal, quickly finding a window with a great view of parked and taxiing airplanes with the assortment of utility vehicles that serve them. He must have stared out for 15 minutes – an eternity for a toddler – watching the busy workers, tiny carts, and giant airplanes zip back and forth on the tarmac.
When we boarded our flight, I was sure to pick a window seat for us, and my wife snapped this photograph of our view after takeoff – sharp, ruffled edges of a large cloud brilliantly illuminated by the setting sun behind it. I remembered my first memories of flying, my own father doing the same thing to make sure that I had a front-row seat to the same spectacle.
But what does this beauty mean to a 15-month-old? My son has so far lived an innocent, healthy life devoid of major trauma or chronic health issues. Though many circumstances are beyond my control, it is among the greatest privileges as a father to provide stability and safety as my son grows and develops. Right now, he knows that the stove makes tasty food, but not that it can burn him. He knows that playing with the garden hose in our backyard is his favorite thing, but not that it’s contingent on next month’s mortgage payment. And I don’t want him to know that the plane he is in might crash, or that the ticket was expensive – I just want him to experience the wonder of viewing a sunset from 30,000 feet. The joys are for today, the burdens for another time.
I moved my face next to my son’s in the window because I, too, wanted to take in the weight of this moment. In the days leading up to our vacation, I was burdened with thoughts of my practice, my finances, my marriage, the hours of sleep I didn’t get the night before, my patients, not to mention the pile of notes that I brought with me from the week prior. What does this sunset mean to me, a middle-aged physician and father? Gazing at the magnificent scene, I couldn’t help but feel that all these difficulties were less important compared to the greater beauty that I was witnessing.
Maybe there are burdens that I, too, am being spared for now, ones that are for the future and not for today. I’m old enough to know that the stove can burn me and that my practice can financially fail. But there are also many more mistakes to make or mishaps to suffer in my lifetime that I have yet to experience, many that I never will. Tomorrow morning, the sun will rise again. Dew will be on the grass, bright red cardinals will roost in my red oak tree, the sky will be blue, and a breeze will occasionally ring my wind chime. Friends and family will still joyfully pick up the phone when I text or call. Spring will follow winter. Morning will follow night. Joy will follow despair. The brilliant cloud commands my attention to this.
And as I gaze back to my left, my son’s feet against my legs while he rests his head in his mother’s lap, I am filled with gratitude and thankfulness. I will carry these burdens with joy and grace. For today, the sunset is enough.
Perhaps, a humbling display of love from a caring Father.
Louis Robinett, MD
lrobinett@rheumtx.com
Submitted June 2025
by Lee Frierson-Stroud, MD

Music-the Soul’s Healer
We have been immersed in the rhythm of life from our very conception. Before we had nerves, ears, lungs—the rhythm of our mothers’ hearts surrounded us, accompanying us on the everyday adventure of becoming human. The lucky were exposed to music in utero. Music served as the soundtrack of our lives. Music is joy and sadness, humble and sublime, solitary and communal. Music is life itself.
Music is also healing. It is a source of endorphins—the good, natural, healthy kind. It is exercise—mental, physical and social. And, it is a gift to oneself, to one’s family and to one’s community.
Many, while growing up, sang or played in school/church choirs or bands. Some learned one-on-one with the piano, guitar, or other instruments. Others hummed and sang to themselves in the car and/or the wonderful acoustics of the shower. Mostly this was placed on the backburner in medical school and residency. We went in hearing one style of music and came out hearing something else. I went in to rock and roll and easy listening and came out to gangster rap and grunge. An elder physician missed the music I grew up to like “Top of the World,” and “Homeward Bound.” But, the call of music was still there.
The joy of music is crucial as one of many ways for physicians to deal with stress. In recognition of this, the Docs’ Noteworthy Ensemble was created. It was the only community choir active during COVID and the only Physicians Wellness Program to remain active in that incredibly stressful time for our physician community. Choral music of all kinds, some sublime (“Ave Verum Corpus”), some just fun (“The Lion Sleeps Tonight”) are featured. Participants are able to rehearse as their schedule permits. Phone calls from patients and colleagues during rehearsal are taken in stride. The idea is to relax as you can. We give back with two concerts per music set—one public with YouTube livestream and one at a nursing home. The archived livestream is available to share with shut ins. We have three concerts (Spring, Fall, and Christmas) per year to keep the music fresh and challenging. The ensemble is made up of singers and instrumentalists.
The audiences are touched by the healing sounds of music and the communal process. The sharing of the gift of music is basic to the human existence.
Thus, whether you love to sing or play music in an ensemble setting, are looking for something to do with one or more members of your family, want to support your musical family member, or if you simply want to go enjoy great live music, come enjoy the Docs’ Noteworthy Ensemble. Our next concert is June 28 at 2:30 pm at the Church at Highland Park, 5206 Balcones Drive (2222/Northland). If you are interested in joining our group or just learning more, contact me at 737-291-3048 or lfsim@me.com. Come join us as we share in the healing rhythm of life.
Lee Frierson-Stroud, MD
lfsim@me.com
Submitted June 2025
by Dr. Sumana Kumarappa, MD

Dancing Through the Demands
A Gastroenterologist’s Perspective on Wellness, Joy, and Preventing Burnout
As physicians, we live and work in high-stakes environments—where our time, energy, and emotional reserves are constantly stretched. Like many of you, I entered medicine out of a deep sense of purpose. As a gastroenterologist, I find meaning in every patient interaction, every procedure, every moment of healing. But over time, I began to feel what many of us eventually do: the quiet creep of burnout.
There were days when I felt like I was just moving through the motions—efficient, focused, but disconnected from joy. The emotional toll was subtle but persistent. I’d come home physically drained, mentally foggy, and somehow still thinking about patients long after I left the hospital. It made me realize something had to change. I needed something that filled me back up.
And I found it through dance.
Dance has always been a part of my life, but recently, it has evolved into something more than a hobby. It’s become therapy, expression, and joy—all rolled into one. What makes it even more special is that I share it with my daughter. We don’t just dance in the living room—though we love those spontaneous sessions—we also perform together with dance teams, rehearse regularly, and even film creative dance videos. It’s become a shared rhythm, a beautiful bond that keeps us both grounded.
In those moments, I’m not “Dr. so-and-so.” I’m not thinking about consults, lab results, or my inbox. I’m fully present—with my daughter, with the music, with myself. That space we create through dance has become sacred. It’s where I find energy again. It’s where I remember who I am outside of my professional role.
These moments are not just fun—they’re deeply restorative. After a week of complex procedures and emotional cases, a few hours of dancing can bring me back to myself. It reminds me that wellness isn’t about escaping the work, but about finding something that fills you up alongside it.
Sharing this joy with my daughter has been especially meaningful. She sees that her mom can care deeply for patients and carve out time for creative passion. She sees that joy and discipline don’t have to be separate. We learn from each other—she brings spontaneity, I bring structure, and together we create something that feeds both our souls.
This connection to dance has made me a better physician. When I take care of myself, I show up more fully for others. I’m more present, more empathetic, and more attuned to my patients. It’s a reminder that we can't pour from an empty cup. Physician wellness isn’t a luxury—it’s a necessity.
I know how easy it is to push self-care to the side. We delay hobbies, postpone rest, and convince ourselves we’ll get to it “after the next shift,” “once this stretch is over,” or “when things slow down.” But things rarely slow down. And we don’t need to earn joy—we need to claim it.
Wellness doesn’t have to mean taking weeks off or making drastic life changes. It can be small, meaningful investments in the things that light you up. Whether it’s painting, hiking, writing, or dancing—find the rhythm that brings you back to yourself. And make space for it, unapologetically.
We hear a lot about work-life balance, but I’ve started to think of it more as life rhythm. Dance gave me that rhythm—something steady and joyful to return to. It’s not about balancing everything perfectly. It’s about creating space for things that matter outside of medicine so we can keep thriving within it.
To my fellow physicians: if you’re feeling stretched thin, I see you. If you’re running on fumes, I’ve been there. You deserve to feel whole—not just as a caregiver, but as a human being. Find what recharges you, and don’t let go of it. That thing—your joy, your creative outlet, your passion—is not a distraction. It’s your medicine.
For me, wellness looks like spinning under stage lights, filming a dance video with my daughter, and remembering that I’m more than my white coat. And that joy? That joy is what sustains the healer.


Sumana Kumarappa, MD
Austin Gastroenterology
sumana.kumarappa@austingastro.com
Submitted May 2025
by Dr. Shangir Siddique

Spring Cleaning Your Roles and Responsibilities
With the coming of a new year, we always have a chance to reflect on what worked and didn’t work in the previous year. In addition to finally cleaning up the mess I ignored while working over the holidays (the hospital never sleeps!), I take a moment to take inventory of something equally important as a clean environment: my obligations and responsibilities. Like many of you, I pride myself on being active in my local medical community and part of the Texas Medical Association. Oftentimes, I’ll take on additional roles and responsibilities outside of my work as a physician, or in organized medicine. It’s easy to forget how you only have 24 hours in a day when during residency, you would often spend most of your waking hours taking care of patients. However, I noticed that it is very easy to have a schedule filled with different meetings, working groups, projects, and roles/responsibilities that individually seem like great ideas, but overall take away from the time I have to myself.
In these fleeting days of spring, take a minute to jot down all of your ongoing obligations, professional, and not professional. Some things are extremely difficult to prioritize as being more important than others but try your best to rank these priorities and obligations from most important to least important. One way to frame “importance” is the impact it has on your well-being. Not only do I consider my work in the TMA objectively important, but I derive a subjective feeling of accomplishment and hard work when I work on a resolution that makes it through the House of Delegates or coordinates with colleagues across the state for ongoing medical issues. To keep it simple, sometimes the work can feel like it’s not work. Prioritize these activities and allow yourself to engage in communities/efforts that bring you a sense of accomplishment and meaning. However, if you find things on that list that don’t provide a sense of accomplishment, don’t provide that sense of impact, or worse, become a negative stressor that isn’t leading to personal/professional growth, ask yourself if you would like to continue to dedicate your limited time and energy towards that effort.
It’s always hard saying no, especially for those of us who entered a field dedicated to healing and serving others. Your impact as a physician will be far greater if you prevent burnout and have a longer career, rather than being overly passionate and stretching yourself too early on and then retiring sooner than you would hope. When transitioning out of a role, I suggest recommending an appropriate replacement if needed. Depending on your role/organization, this may allow for a positive career trajectory for that person, while also establishing yourself as a team player who wants the overall team to succeed.
Taking this approach has allowed me to focus on being effective and efficient with my roles and responsibilities, while also nurturing a strong network of colleagues who I can always reach out to for their advice and perspective. I hope this spring brings you much growth and abundance!
Shangir Siddique, MD
ssiddiquemdmph@gmail.com
Submitted May 2025
by Dr. Michelle Owens-Kumar
A Moment’s Grace: Navigating Medicine & Motherhood
Being a physician mom is a juggling act like no other. I knew it would be hard, but I never imagined just how much. The guilt, the exhaustion, the constant pull between caring for patients, leading teams, and showing up fully for my children—it’s overwhelming. And yet, in the chaos, I’ve learned one of the most valuable lessons: give yourself grace.
Before motherhood, I thought my medical training in family medicine would prepare me for parenting. I couldn’t have been more wrong. From the struggles of childbirth and breastfeeding to the brutal reality of functioning on minimal sleep, I pushed through, often too hard. Looking back, I wish I had been kinder to myself. I wish I had whispered, It’s okay. Ask for help. Take a break. The notes can wait. You are doing an amazing job.
Now, I try to be more mindful of my inner critic, to set and hold boundaries, and to remind my colleagues to give themselves the same compassion they so readily give to others. I’m far from perfect, but I’ve grown. And when I struggle, I ask myself: What would I tell my daughter if she were in my shoes? The answer is always gentler, always more forgiving.
The other day, my 6-year old daughter told me that when she grows up, she wants to be a veterinarian, an artist, and a mommy. Then she looked at me with wide, curious eyes and asked, “But mommy, how do I do all those things at once?” I had never felt so seen. I paused, unsure of the perfect answer, and said gently, “You do the best you can in each one, knowing you have to take time for each—and be kind to yourself, because you can’t do everything at the same time.”
Recently, I chatted with a colleague, and we shared how there is so much overlap between our personal and professional lives as mothers, doctors, and leaders. Our doctoring shapes our mothering, our mothering strengthens our leadership, and our leadership informs it all. But too often, we forget the grace we need across all three roles.
I wonder what it would be like if we scheduled moments of self-kindness each day. What if we paused long enough to honor all we’re doing instead of focusing on what we’re not? What if we allowed ourselves, just for a moment, to step away from the hustle and simply be—without guilt or expectation, and just with grace?
As we strive to be well-models for the next generation, I hope we also remember to extend that same kindness to ourselves. You are doing enough. You are enough. Give yourself that grace.
Michelle Owens-Kumar, DO
mowensdo@gmail.com
Submitted May 2025
by Natalie Malluru
The Unseen
In sterile rooms where echoes swell,
Between the charts, the notes, the tell
A quiet battle, buried deep,
Where shadows lurk, and secrets keep.
What weighs upon the hands that heal,
When pain is real but stays concealed?
A spectrum cast in muted tones,
Yet thrumming loud in weary bones.
Each breath of anguish, thin as air,
Felt so sharp, yet never there.
In jaded eyes, a fleeting fear
Will my truth be lost, unheard, unclear?
This world of science breaks and mends,
It measures wounds, yet not the bends
Of spirit twisted, pulled too tight,
A silent war still out of sight
But look beyond what scans reveal,
Beyond the proof, beyond the steel.
See the weight, the quiet ache,
The fight they fight but cannot break.
So fear not the edges, let them blossom and grow,
Each thread of existence is vital to show,
In this clinic of hearts, understand what they bear,
Dissolve doubt that lingers, and breathe in their air.
Together we navigate this invisible tide,
Charting paths of resilience, with you here beside,
In the fabric of healing, let patience be bright,
Let us honor the pain, transform darkness to light.
Author’s Note
"The Unseen" depicts the challenges encountered by individuals suffering from invisible illnesses, such as fibromyalgia - a complex condition that is often overlooked or misunderstood. It captures the internal struggle of patients whose suffering is real yet elusive in the eyes of modern medicine. The lines convey a sense of isolation as patients battle not just the physical aspects of their illness but also the pressure to prove their pain. These writings stem from wanting to honor the unseen and are inspired by my time rotating through fibromyalgia clinic.
Natalie Malluru | MD Candidate, Class of 2025
nataliemalluru@utexas.edu
Submitted April 2025
by Robina Poonawala, MD

WHAT IS HAPPINESS, REALLY?
Happiness is the elusive butterfly we all chase, hoping it will land on our shoulder someday.
But what is happiness, really? Is it a feeling, a destination, a skill or a state of mind? Does it come from fancy titles or free time?
The modern workplace is designed for efficiency, not joy. The employees are given targets, not indexes for happiness. Imagine a world where companies offered “happiness bonuses” instead of “performance bonuses.”
Psychologists say happiness is 50% genetics,10% circumstance and 40% mindset. So, if you were born into a family of worriers, you are halfway to anxiety. The remaining 50%? Well, that is where the magic lies.
Social media has redefined happiness. A vacation is no longer about relaxation but about curated Instagram posts. The pressure to appear happy has taken over the need to be happy. And let’s not forget about consumerism’s goal in happiness. Advertisers have convinced us that happiness can be bought - the right car, the right watch, the right perfume. But as the saying goes, ‘money cannot buy happiness,’ but it can sure buy a yacht, private jet, or a thing or two.
Neuroscience tells us that small joys release dopamine, serotonin, and oxytocin–the holy trinity of happiness. It’s why a Frappuccino, a dog’s wagging tail, or a smile can brighten your day. A smile can trigger another smile, creating a ripple effect.
We often forget that happiness and health are two sides of the same coin. You can have all the wealth in the world, but if your back cracks louder than your most comfortable chair, joy feels distant. A balanced life is not about financial success, but physical and mental well-being too.
The irony is we spend our youth chasing money at the cost of heath, only to spend that money later trying to regain it. We treat happiness like a pension plan, deferring it for later, believing things like, “I’ll be happy when I get a promotion,” or “I’ll be happy when I buy that dream house.”
But happiness does not come gift wrapped with a milestone. Happiness is not a future event; it’s a present choice.
The key criteria for happiness generally include financial stability, strong relationships, good health, and a sense of purpose. Money can provide happiness by providing basic needs and security but beyond a certain income level, additional wealth has little impact on long term happiness. More important are strong personal connections–family, friendships, and community. Good physical and mental health play a significant impact on happiness as does having a sense of purpose whether through work, personal growth, or helping others.
Ask a child what makes them happy and the answer will be simple; an ice cream cone or picking up seashells on a beach. Ask an adult and the answer will be a complicated mix of ambitions, financial stability, and societal expectations. Somewhere along the way we stopped living in the moment and started living for the future.
In summary, let's recognize that happiness is not a luxury, it’s a necessity. It is not found in grand achievements but in small, everyday moments. True success does not lie in reaching milestones but in savoring the journey. A world that prioritizes happiness is a world that thrives, and perhaps the real measure of success is not how much we have accumulated, but how much joy we have created–for ourselves and those around us.
Robina Poonawala, MD
robina.poonawala@gmail.com
Submitted March 2025
by Louis Robinett, MD

Is this it?
A couple of years ago, an acquaintance of mine from medical school posted a series of concerning posts on his Facebook profile. I reached out via Messenger, and we had a brief conversation that revealed he was not doing well. He had just completed extensive post-graduate training as a surgical subspecialist. He had a beautiful family, and he bought a lovely home in the town where he settled as a respected member of the medical community. From a career standpoint, he had finally made it. So how in the world could someone in his position be depressed? It seemed that he was wondering the same thing.
I have witnessed this pattern in a number of friends and patients, and while the process may differ for each, the result is the same. A physician finally makes partner, a young professional lands that coveted job at a flashy company, a stay-at-home mom’s children finally leave the house and she finds herself at loose ends. After years of labor, you finally achieve your goal, and yet find yourself asking the question:
Is this it?
I recently saw a Reel of an interview of Jason Alexander, the actor who played George Costanza in Seinfeld. He told a story of finally winning a Golden Globe award after a lengthy career of hard work. Despite how incredible the moment was when given such a great honor, when the ceremony and after-party were over he got back to his hotel room and found himself surprisingly disappointed. “Is this what it feels like to be at the top?” he thought. He wished he had taken the time to enjoy the process and had a more realistic expectation of the destination.
There are similar realities in the field of medicine. I was struck early in my career how much the day-to-day work of a doctor felt more like a normal job than the fulfilling ministry I had envisioned in my pre-med days. Our patients commonly have the same mindset, treating our interactions with them as a transaction, not appreciating the weight of responsibility and beneficence we feel for them. Much like the story of Jesus healing the ten people with leprosy, only one came back to say, “Thank you.”
Being no stranger to these feelings myself, on bad days I feel like clinical practice does little more than just punch my paycheck. But I have to remind myself that this is only a portion of the totality of work that I do. No vocation is absent of frustrations or repetitive tasks, and I must accept those along with the joys and rewards that come with them. It is also important to remain thankful in all circumstances – our human nature naturally focuses on problems and suffering instead of realizing gratitude. I have a recurring monthly email I schedule to myself to remind me to, “Be thankful for both the blessings and challenges of this season.” I started this a year ago during a particularly stressful time at my practice. And finally, according to my Christian worldview, I try to remember that my identity ultimately lies with God’s perspective of me, which is independent of performance, successes, or failures – a concept that I all-too-easily forget.
From one physician to another – thank you for what you do. Remember that all our work is meaningful, even when we feel like it isn’t. Each mundane task (does anyone enjoy writing notes?), challenging diagnosis, and successful treatment helps to improve the health and lives of our patients. If indeed, ‘this is it,’ be encouraged that you are making a difference in the lives of others and know your colleagues (and even your patients) see your worth and value.
Louis Robinett, MD
lrobinett@rheumtx.com
Submitted March 2025
by Michelle Owens-Kumar, DO

Sing Sweet Nightingale: What a Lullaby Teaches Us About Physician Well-Being
As I sing this song at bedtime to my youngest, I wonder what about this song, in particular, is so comforting to him. Is it the melody, the familiar voice, or the cadence of the words? Did watching Cinderella with his older sister really leave this strong of an impression?
As I thought of it more and researched the meaning behind it for myself, I was pleasantly surprised to find that this song has often been viewed as a beautiful escape for Cinderella from her unfortunate circumstances—an attempt to preserve her mental well-being despite the adversity she faced.
In fact, the nightingale has often been seen as a symbol of strength, hope, and healing. In literature and mythology, the nightingale’s song has long been associated with solace in times of sorrow, a reminder that beauty and light can exist even in the darkest moments. For physicians, who often bear the emotional and physical toll of their profession, this symbolism is particularly poignant.
Much like Cinderella seeking refuge in her song, many healthcare professionals turn to moments of reflection, music, or personal rituals to maintain their well-being amidst the demands of their work. The nightingale, often a metaphor for endurance and renewal, reminds us that tending to our own mental health is not just necessary but vital in sustaining our ability to care for others.
But beyond just seeking comfort, we must also recognize the importance of channeling our inner strength during difficult times. Struggle is inevitable in medicine and in life, but unnecessary suffering comes when we resist what we cannot control or when we neglect to replenish ourselves. True resilience is not about enduring hardship in silence—it is about knowing when to pause, when to seek support, and when to lean into practices that nourish us rather than deplete us.
I find myself reflecting on the ways in which we, as physicians, can create our own moments of respite—whether through music, mindfulness, or simple acts of self-care. Just as the nightingale’s song provided Cinderella with a sense of peace, we too must find our own melodies that sustain us, allowing us to navigate the challenges of our profession with grace. In doing so, we not only protect our well-being but also ensure that we can continue to show up fully for our patients, our loved ones, and ourselves.
Michelle Owens-Kumar, DO
mowensdo@gmail.com
Submitted March 2025
by Scott Clitheroe, MD

A Kind Gesture
In 1990, on the internal medicine wards at Hermann Hospital in
Houston, Texas, it was (morbidly) joked that there were three types of
inpatients: those with AIDS, those with tuberculosis, and those with both.
It was to these wards that I was assigned as a third-year
medical student on my internal medicine rotation. I was nervous. The patients
with AIDS were numerous and very sick. The medical student duties included
drawing blood cultures on patients that spiked fevers. Needle sticks were a
constant concern to us novice phlebotomists.
Early one evening, my supervising resident told me to draw blood
cultures on a patient who was spiking a high fever. He was a middle-aged
Haitian immigrant admitted with AIDS-related Pneumocystis pneumonia. Despite
appropriate treatment, he continued to spike fevers, so blood cultures were
ordered.
When I entered the room, wearing my mask and isolation gown, I
was met with a kind smile from a gaunt man. I introduced myself and told him
that I needed to draw blood from both arms. Like a supplicant, he outstretched
both his arms and said I could join the crowd of vampires.
I perspired under the heavy gown. I also was hungry and probably
hypoglycemic, as I hadn’t had time to eat lunch or dinner. I guess I looked
peaked, because as I was preparing to draw the blood, he asked me if I was
feeling okay.
Taken aback by the question, I murmured something about being
hungry because I had skipped lunch. I didn’t want him to think I was nervous
about the procedure. He replied that I shouldn’t be skipping meals, because
learning was harder on an empty stomach. I nodded in agreement, finished the
blood draws, thanked him, and left the room.
The next morning on rounds, one of the ward’s nurses told me
that the patient asked to see me. I had not been assigned to his case; I had
just been there to draw blood. So, I was confused as to why he would want to
see me.
When I entered the room, he motioned me over to the bed and the
bedside table, where his breakfast sat uneaten. On it was a wrapped muffin and
a ten-dollar bill. He insisted that I take the snack and the money. He had
assumed that the reason I had skipped meals was not due to lack of time, but
lack of funds. I was blown away by the generosity of a man, dying alone in a
foreign country, who was still able to think of others’ needs.
I thanked him and tried to correct his assumption, but he
insisted. Finally, I acquiesced and took the muffin and the ten-dollar bill and
left the room. That muffin tasted really good, and I used the ten-dollar gift
for both lunch and dinner that day.
I stopped by his room the next day to thank him. He clearly was
not feeling well but he managed a smile and a few kind words. I never saw him
again. He passed away a few weeks later.
When I am feeling stressed, sad, or scared, I often recall the
kind gestures of a dying patient and remember that the best remedy to these
common human emotions is to serve others. In that service, we can begin to
realize that the travails we encounter are not ours alone; that we humans are
all in this together.
What a blessing it is that we chose a profession where we are
privileged to be in service to others every day.
Scott Clitheroe, MD
sc51806@gmail.com
Submitted March 2025
by David Fleeger, MD
Just Get Away
I’m not exactly the poster child for work-life balance. So, when asked to post some musings about handling the inherent stresses of our profession I was a little suspicious they were going to use me to demonstrate what not to do. After all, our Travis County Medical Society already does a sterling job in providing resources to our physicians and their families who feel overwhelmed in their daily lives. If you feel in need of these services, your colleagues, friends, family and coworkers ask that you take advantage of the TCMS Physician Wellness Program counseling sessions. We want you whole and healthy.
Having worn a few hats in my medical career I have certainly seen my fair share of highs and lows, both in day-to-day patient care and in the political machinations faced by our profession. And like most, I have been helped through these days by my faith, family, friends, and coworkers. The pearl that I could pass along to my fellow physicians is to just get away. Both mentally and physically – just get away. For me, that means often combining two passions: photography and travel.
Photography has been an interest since residency, but it wasn’t until I entered practice that I began to seriously study, upgrade my equipment, and practice, practice, practice. I think the surgeon in me appreciates the technical aspects of the art and the ability to achieve a sharp and properly exposed image in an endless variety of circumstances. At the same time, the artistic side of photography is the most challenging. It’s not just a matter of good subject, light, and composition. It’s being able to use these to tell a story, to move someone – to capture a moment that has that ‘wow’ factor. This is the aspect of photography that you can work on for a lifetime and always have room for improvement.
The other passion that I share with my wife Jamie, is for travel. Although we have had many great trips within the USA, we decided early on (in our more mobile years) to get as far away as possible. I enjoy reading about the history and culture of an intended visit, as well as the geography, wildlife, and (of course) the photographic opportunities. Although travel these days can be a little stressful, we have learned to do our best to prepare and then just take things as the come. We did spend a Christmas in New Zealand without our luggage, but this gave us an excuse to buy a bunch of new clothes. Once in the country we try to immerse ourselves in the culture and experiences of the day-to-day lives of the locals. We prefer local guides and stay in locally owned hotels when possible. With a smile on my face and camera in hand I have met Buddhist monks in Bhutan, retired nuclear physicists in Cuba, and an Orthodox Christian priest named Paul in Patmos. For me the perfect location has no cell service and shoddy internet. I don’t bring any work with me. If I am doing it right, I don’t even think about work after two or three days. I will get my head back in the game and clear my emails out during layovers on the way back.
The combination of a technical skill that requires significant focus and the excitement of a strange and wonderful environment allows me to clear my head, forget about work, and create lasting memories with family and friends. The point is to both mentally and physically go somewhere entirely different from home. I know I have succeeded if when I get back to the office, I can’t remember my EMR password. So do yourself a favor and just get away.
David Fleeger, MD
davidfleegermd@austin.rr.com
Join me on Facebook for my Photo of The Day, click here






Submitted March 2025
by David Fleeger, MD
Submitted March 2025
by Dr. Christopher Parker
Doctoring and Learning: The First 25+ Years
July 1, 1997 was one of the best days of my life because I became a rheumatologist. I love caring for patients with multisystem autoimmune and crystal illnesses. Most of the time I am doing the teaching and coaching, however as a lifelong learner, staying abreast in medicine is always a massive challenge. I have always found it delightfully valuable to learn from my patients. Learning from patients often diminishes my stress regarding things like wrestling with insurance and other administrative hassles.
Here are a few keys to health and happiness my patients have taught me in their words:
1. From the late 70s guy who rides his motorcycle more than 100 miles to me once a year to refill his gout medication and Viagra. The keys to good health are, "Grow old but not up" and "try to eat less and have sex more".
2. From a 90s-year-old man I followed for decades with rheumatoid arthritis who always had a smile, even on the day after his daughter passed away from breast cancer: "I am so lucky to have known her for 44 years."
3. From a 60s-year-old lady who had very refractory rheumatoid arthritis: "I just need to laugh or cry, so I’d rather laugh." She would muster a smile and giggle. I would tell her that if I were her, I would sing the blues. She would often giggle again and say something like, "Then I
would cry since I'll bet you can't sing" and then we would both laugh.
4. From Freddie, a 90-year-old who I took care of for at least 20 years: "Always have the kind of job you would want to do in retirement."
5. From my patient's husband who came to see me in clinic a year after her death carrying a framed picture of her when she was a young lady: He wanted me to know that in her younger years she was very beautiful compared to the last few when I knew her. Then he pulled
out the letter of condolence which I wrote right after her death. He had been carrying it around in his wallet all of this time and wanted me to know "this meant a lot to me." It still chokes me up when I think about it.
Yes, there are words of wisdom here, but I find the true joy of medicine is within human connections and sharing whatever we can to lighten the burden of the human condition.
Dr. Christopher Parker
dr.positiveparker@gmail.com
Submitted February 2025
by Dr. Michelle Owens-Kumar

The Amen Effect: Honoring Our Own Suffering to Heal the Healer
In medicine, we bear witness to suffering daily—our patients’, our colleagues’, and our own. This has been magnified over the last few weeks as we are navigating uncertainties and change. The weight of this responsibility can be immense, making it all too easy to either become overwhelmed or emotionally detached. Rabbi Sharon Brous, in her recent book The Amen Effect, reminds us of a powerful alternative: to honor suffering, move through it, and embrace healing as a communal act. She talks about not only bearing witness, but also bearing with-ness, to highlight the importance of maintaining connection during difficult times.
Through a series of relatable stories in the Amen Effect, Brous describes the act of showing up for one another in moments of pain and joy, acknowledging suffering rather than turning away from it. She describes an ancient pilgrimage ritual where hundreds of thousands of Jews would travel to Jerusalem to climb to the Temple Mount plaza where they would turn to the right to circle counter-clockwise. Those who were grieving, lonely or sick would embark on the same journey, however, once they reached the plaza they would turn left to circle in the opposite direction. As each person traveling right passed a bereaved, sick or lonely person, they would pause to look them in their eyes and ask "What happened to you? Why does your heart ache?" This practice allowed the mourner to share their pain, to feel seen, and then to receive a blessing validating that they are not alone in their suffering; in fact, they are surrounded by community. This beautifully illustrates the power of connection and our common humanity. This principle is vital for physicians. We are often so focused on healing others that we neglect our own need for support, reflection, and restoration. But true strength doesn’t come from avoidance—it comes from facing hardship with openness, processing grief and stress, and finding ways to replenish our own spirits.
As healers, we must allow ourselves the same grace we extend to our patients. This means seeking out supportive communities, engaging in meaningful reflection, and embracing practices that sustain us—whether through mindfulness, connection, or simply giving ourselves permission to feel. Honoring our own suffering is not a sign of weakness but a step toward sustainability in both medicine and life.
This week, consider where you can acknowledge pain, show up for yourself or a colleague, and create space for healing. Only by tending to our own well-being can we continue to care for others with presence and compassion.
Dr. Michelle Owens-Kumar
mowensdo@gmail.com

Submitted February 2025
by Richard DeBehnke, MD
Medicine’s True Work: Building Trust
As I prepared to step away from the active practice of medicine, I was asked to provide some perspective on my journey. Ask my family, my peers, and my patients and they will confirm that I am more than willing to share.
Perspective tells me that we are not in the business of diagnosis, treatment, or procedures but that we are in the business of trust.
This is curious to me because my medical training never emphasized trust. It was my experience that the opposite was encouraged: C.Y.A. Instead, the emphasis seemed to be on ordering an excess of labs, never admitting a mistake, and in general doing anything and everything to avoid malpractice claims. Our patients were known as “heart failure in room 207,” effectively reducing someone’s loved one to an ICD 10 code. But we were smart, we were committed, and we took care of people.
As my career progressed, I struggled with finding the most efficient way to persuade patients that a course of treatment was necessary, reassure them while they were suffering, and help them accept the reality of their illnesses. How could one best take their knowledge and skills and do some good? In day-to-day practice how do you find success and reward in what you do?
I do not have answers, but it seems obvious to me that trust is involved. Without it, medical care seems impossible. Miraculously, trust seems to exist, but where did it come from and what did I do to deserve it from my patients?
How do you get someone to trust you?
Hemingway was quoted as saying, “The best way to find out if you can trust someone, is to trust them.” It is humbling to realize the people that step into our exam rooms do just that. They take a chance on us. How did we earn this generous gift? By being right all the time, curing every illness, or performing procedures no one else could do? We know this is not what happens. What are the step-by-step directions to acquire this ability, the conscious changes to make, or the places to go to uncover these mysteries? Can any of us say when it happened? Was it always there?
The other side of this beautiful dynamic, which rewards us as much or more than it does our patients, asks: If we are trustworthy, are we trusting? If our patients have the traits of a trusting person such as reliability, patience, openness, vulnerability, and honesty, do we share the same traits? Are we as open and vulnerable with them as they are with us? Can we really care for anyone without making that connection of trust, letting them know that not all of our experience comes from textbooks or seminars, but from walking the same paths that they have? Are they really just looking for a partner to walk the road with them, guiding them around most (but not all) pitfalls, and being there to help them up when they stumble? From these fellow travelers we receive the thanks, loyalty, and respect that make our work meaningful. Reflecting on all the books we have read and shows we have seen, haven’t we sat in rooms and heard real stories just as dramatic and poignant? “Can you help me?” may be the highest praise one person can give to another.
I believe what is most important to the people we care for is not getting it right but getting them.
Finishing this I am struck by the number of questions I have asked, so obviously this is not a guide or set of instructions. But I am confident in saying that we are purveyors of trust, and I encourage you to open up and trust your patients, your peers, and most importantly, yourselves. Perhaps all this is just a personal reflection on my career. If so, I hope reflection implies that a little light and some focus has been generated along the way. That would be good enough.
Dr. Richard DeBehnke
debehnker@gmail.com

Submitted February 2025
By Lauren J. Crawford, MD
Moving Meditation & Revisiting Fight Club
Fight Club is a 25-year-old movie that is raw, irreverent, thought provoking, and clumsy. For me, it’s also nostalgic. Movie magic for a college student. I watched it again recently. The movie still resonates but for different reasons and through the lens of an older eye.
I’ve been asked twice to write for our wellness group. I give a wry smile and say ‘Sure!’. The truth is that I’m not good at wellness. I’m like a wellness dropout. I’ve done one therapy session in my life after my mom died and I found it awkward and hard to focus. I stupidly can’t meditate, and a long session of gentle yoga has the opposite effect of what’s intended.
But I’m good at looking at a hectic physician’s life and figuring out how to lighten the load and make it easier. Working to build egalitarian households, spending money wisely to offload home stressors, and saying no to unsustainable workplace practices are the big ones. Making life easier before you not just burn out but absolutely flame out. I have learned a few things in 15 years of practice.
Another big one – carve out time for your fitness and do not ask for permission to do so. Your kids will be fine. Let them have 30-60 minutes of a 1980’s childhood. Spoons will go missing. A giant hole will get dug in the backyard. They’ll probably live.
I learned a phrase about wellness where I found success and it stuck with me. Moving meditation. It’s the best tool in my toolbox for making me feel well. And, I bet I’m not alone. I’d also be willing to bet that there is a form of moving meditation that helps everyone. You just have to find your own groove.
For me its running and sometimes running to near exhaustion. Don’t worry folks, I don’t do this on OR days but all the other days are fair game. This is where my interest in Fight Club resurfaced.
I am Jill’s hypothalamus. Although I can enjoy it, walking doesn’t work for me. Running a moderate pace helps me focus on a problem and work on solutions because it dims the peripheral noise. Running hard or super long makes everything go quiet and primal. Maybe it’s because my body is so focused on surviving it. Maybe it’s the endorphins and other neuro signaling. It’s such a nice feeling to tune out all the noise except the immediate environment, my feet moving, and my muscles complaining. It depletes creative thoughts, but also the malingering worry. I sleep hard.
‘No distractions. The ability to let that which does not matter truly slide.’
I don’t look good either. I look basic and sweaty. Sweaty in a gross way, not in the rich pine-smelling sauna way. It’s good to lean into that every now and then when the world around us constantly creates content to help us approach perfection. It may be strange to hear this from a plastic surgeon but even plastic surgery doesn’t get you there. Lighting, makeup, filters, angles. It’s good to just exist in your skin and let yourself be imperfect.
‘After fighting, everything else in your life got the volume turned down.’
After the run, the effect does hold. After something challenging, I’m physically done but also the most mellow soul in the world. Beer thirty with no beer. Consistent work really infuses that mental Zen into my life and my personality takes a dive when I can’t do my thing. I don’t think this is something that science has a good understanding of although we know that exercise can occasionally outperform meds and therapy for depression. For doctors, I think it can temporarily drown out the bad clinic experiences, the frustration with an administrator, and even just the busy worker bee mentality to constantly chase productivity. We all need breaks even if we can’t find all the solutions in a day.
‘Being tired isn’t the same as being rich, but most of the time it’s close enough.’
I encourage everyone to find something relatively intense that uses their body that they hopefully like to do. Dirty minds may go where they wish. For others I imagine it could be dancing. The kind of dancing where distraction means you end up on the ground. Challenging rowing, yoga, rucking, or actual boxing. Choose your own adventure. But it has to be accessible and not a novelty because you have to do it with some frequency. And, you have to mostly like it. After 8 or 12 weeks, maybe it’s a habit.
Good luck with your very own moving meditation. Maybe a skosh less intense than fight club and with a side of better coping strategies. I highly recommend it.
Signed,
Jill’s Prefrontal Cortex
Dr. Lauren J. Crawford
laurencrawfordmd@gmail.com

Submitted February 2025
By Dr. Tina Philip
Change
“In any given moment we have two options: to step forward into growth or step back into safety.” - Abraham Maslow
For as long as I can remember, change is something that I have dreaded. I have always been a creature of habit and am most comfortable in my predictable routines. I wouldn’t consider myself a highly anxious person, but I definitely experience some apprehension when things don’t go as planned.
March 16, 2020. Most of you probably remember this time frame as when the pandemic became a reality for us here in central Texas. I remember this specific date as the day I opened the doors to my brand-new solo practice. Four days later, those doors “closed” as shelter in place orders went into effect. Talk about things not going as planned.
For many years prior, I had thought about changing my practice situation. I began to interview for other jobs, but I was fearful of change. What if a new job is worse than the one I already have? I did interview after interview, finding fault with each one because it was not exactly what I wanted. I realized that if what I wanted did not exist, I would have to create it myself.
Then the fear of starting a practice set in. What if I failed? What if it was too hard? I began the arduous process of building a practice. There was a cautious optimism as I started to make decisions on what my future practice would look like. Each step away from comfort was a step in the right direction, even if it did not feel like it at the time. Of course, planning for a global pandemic was not part of my business plan, but as it is with many other challenges in life, I rolled with it. It was daunting opening a new practice amid such uncertainty, but I was determined to press forward despite the challenges.
As you read in last week’s Sunday email, Dr. Brian Sayers has stepped down as chair of the Physician Wellness Program. When I first read it, I had a lot of feelings, the main one being sadness. In the TCMS Physician Wellness Program he has created something unique, the likes of which cannot be replicated, and for that, I cannot thank him enough. In a time where so many of our social connections seem superficial at best, the multiple facets of PWP have created tethers to something real; something that reaches the humanity of being part of this family of medicine. He has put himself into this program in more ways than any of us can fully understand. How can this program possibly continue without him in charge?
Then the reality of assuming care of this program in the interim set in. There is a lot of fear attached to taking responsibility for something so important to so many people and trying to fill some very big shoes. What if these emails stop speaking to people? What if I mess up this program? What if this program loses its spark? The answer to such natural worries is that our efforts will be guided by the TCMS Foundation board, and the program will continue, perfectly or imperfectly, to focus on the many needs of physician well-being.
I fully believe that everything happens for a reason and in its own time. As uncomfortable and unwanted as it is, change is necessary for the growth of this program. Maybe the point is not for the program to continue to exist as it is, but to continue to evolve and support the needs of our ever-changing physician community. Ultimately, while the Foundation board is its steward, the Physician Wellness Program belongs to our physician family. Although it will not be the same as it was under the familiar warmth of Brian’s leadership, I am cautiously optimistic that it will be what we need, because we will grow it together.
Tina J. Philip, DO
President, TCMS Foundation Board
tina.philip@gmail.com

Submitted January 2025
By Dr. Brian Sayers
Pilgrimage
In 1969 ethicist Paul Ramsey delivered a series of lectures sponsored by Yale Medical School and Yale School of Divinity, later published and widely disseminated, ushering in the era of modern medical ethics and bioethics. I came across my copy of it recently, dozens of Post-It tabs highlighting specific areas that meant something to me when I read it more than a decade ago in seminary. One particular line has always stuck with me: “The practice of medicine is one such covenant. Justice, fairness, righteousness, faithfulness, canons of loyalty, the sanctity of life, hesed, agapé or charity are some of the names given to the moral quality of attitude and of action owed to all men by any man who steps into a covenant with another… explicitly acknowledges that we are a covenant people on a common pilgrimage.” Whether viewed through a religious or secular lens, the idea is clear and gives us an admittedly idealized view of the doctor-patient relationship.
It got me thinking about the nature of the doctor-patient relationship. This partnership is critical to keeping both patient and doctor emotionally healthy and keeping both fully engaged in achieving optimal medical care. But this relationship can be a moving target in a rapidly evolving healthcare environment with the rise of medical consumerism and the ease at which our patients can research and become more active participants in medical decision-making. Described another way, “this relationship has been profoundly shaped by the human rights movement of the past several decades, and clinical care today is guided by norms of shared decision-making rather than benevolent paternalism.” Understanding, honoring, and navigating each individual patient’s desires and understanding of this relationship is critical in a working partnership with patients. Emphasis is now usually placed on patient satisfaction within this partnership, often emphasizing the physician’s bedside manner, but increasingly we also realize the importance of this relationship to the health of the physician. In the end, we will all have played both the role of physician and patient.
Defining the key elements in bedside manner is often made more complicated than it should be. A group from Harvard Medical School described 4 key components: trust, knowledge, regard (friendliness, warmth, emotional support), loyalty. More recently, a great deal of emphasis has been placed on the level of empathy that is both heartfelt and tangibly evident when a physician cares for a patient. There is great truth in this: a sense of understanding, of “shared suffering” is indeed what we all need to different degrees throughout our lives. In his landmark article, “The Nature of Suffering and the Goals of Medicine,” Eric Cassell notes, “the relief of suffering and the cure of the disease must be seen as two obligations of a medical profession that is truly dedicated to the care of the sick.” Others have noted that although empathy is an essential characteristic of a holistic physician, it can be a two-edged sword that, when unbalanced or overdeveloped, can affect objectivity, judgement and can be a significant contributor to physician burnout.
A more basic understanding of the relationship between physicians and patients might just involve kindness. Kindness is hard to define, but easy to recognize. When you think about it, kindness encompasses all the critical components of covenant that Ramsey spoke about at that gathering of great minds a half century ago. The more I have thought about kindness and now try to write about it, the more I realize how far short of it I fall most days, and how often I see and admire it in my colleagues, including my own doctors. It’s easy to find yourself in a hurry or frustrated or distracted and fail to see the shared humanity, even suffering in its many forms right there in front of you and to fully honor that covenant, that common pilgrimage physicians and patients take together. Perhaps intentionally honoring that high calling more often than we miss, it might just be the difference between loving our work and just having a job.
The legacy that we slowly mold, then leave behind after a long, or even a short, career in medicine may in part be defined by our diagnostic or therapeutic acumen, but when I consider my colleagues, past mentors and teachers, I think it is defined in a more lasting way by the characteristics that bond us with our patients and colleagues − patience, fidelity, empathy, love, but especially kindness. Yes. Kindness. That just might be enough.
Brian Sayers, MD
Chair, TCMS Physician Wellness Program
Contact Dr. Sayers at briansayers24@gmail.com

Submitted January 2025
By Dr. Robina Poonawala
The Truth about Penguins and Doctors
A sprawling city bustles with the loud racket of morning hour rush. Crowds of commuters hurry past each other. Suddenly, one traveler bumps into another and sets off a shouting match.
This might seem like a typical morning in New York City, but the location is Antarctica and these commuters are chinstrap penguins. Named for facial markings that resemble helmet chinstraps, these flightless two foot tall birds live in and around Antarctica and nest in crowded communities called colonies. Many chinstrap colonies are home to hundreds or thousands of individuals and have a lot in common with manmade urban centers and their inhabitants.
Every November near the start of summer in Antarctica, chinstrap penguins arrive at their breeding grounds. There, they begin construction work. Mated pairs use pebbles to build nests that are up to 20 inches wide, like human neighborhoods arranging their nests side by side. They live in close quarters for safety ‒ a lone nest would be a sure target for skua, a predatory bird that swoops from the sky to snatch chinstrap eggs or chicks.
While penguins have evolved from flying birds, their superpower lies in being the best divers of all birds. To protect from the cold, they have dense feathering, and different species are distinguished by the colors of their heads. Female penguins lay one or two eggs and both parents take turns caring for the eggs. While one stays behind to keep the eggs warm and safe from predators, the other heads out to sea to feed on krill, fish, and squid. Once hatched, they are carefully watched for around three weeks when both parents may have to leave to forage for food while their chicks gather in the safety of the larger group of other young penguins called crèches for warmth and protection. This shared labor is so important that a penguin chick will not survive if it has only one parent. Chicks who are hungry may beg from other parents but there is no fostering, and adults will only feed their own offspring.

By March, when the chicks are nine weeks old and their downy baby feathers have been replaced by waterproof adult feathers, they plunge into the sea and forage for their own food. Mated penguins use calls to identify each other and their offspring. The penguins are monogamous and return to the same breeding partner year after year. As far as scientists can tell, there are no couples therapists or divorce attorneys in the colonies.
Observing penguins reminded me of the importance of community. We all need connection with each other for communities to survive and prosper and for our children to thrive in their formative years.
We feel security and a sense of contentment when we are with our peers ‒ the human version of the warmth and security that penguin communities model. Just as the penguins huddle together to survive harsh weather, shortage of food, and predators, together in community physicians and their families survive and thrive in spite of a wide variety of challenges, even predators, that we face daily as individuals and as a profession. We just have to stick together!
Dr. Robina Poonawala
Send comments to Dr. Poonawala at robina.poonawala@gmail.com


Submitted January 2025
By Dr. Brian Sayers
Real Change
When this comes out on January 5, there’s one thing we can count on: most New Year’s resolutions have already been abandoned. New Year’s resolutions fail because they are usually quick fixes for bad habits or other problems that involve a solution that is no fun and that we aren’t really all that serious about, often changes that involve weight, exercise, diet, alcohol, or spending. The plan, if it can be called that, typically overestimates the effectiveness of willpower, of muscling through a firmly entrenched behavior pattern, often ignoring the reality that change requires not just bulldozing over entrenched behavior, but actually understanding the behavior and why it makes us unhappy even as we persist in doing it. What some authors call “real change” is, well, real hard. It involves the big things in our lives that stand in the way of contentment, meaning, or honoring our deepest beliefs.
Real change isn’t hatched in a vacuum. It is usually a response to a sense of unease or sadness or yearning. The spark that starts the fire can be anger, grief, regret, shame/guilt, bad habits/addiction, relationship problems or loneliness. Each of these are serious internal feelings that must be explored, their roots understood for lasting change to be possible. One of the most rewarding aspects of working with physicians in PWP these last few years has been to witness and fully appreciate our capacity to make meaningful change. We see it in a variety of life-changing expressions − in committing to recovery, in reclaiming their calling by changing their practice setting mid-career, in seeking counseling, and sometimes by either saving or stepping away from a failing marriage. Willingness to change is an essential part of any life, but not an easy one. Theologian and ethicist Reinhold Niebuhr once noted, “Change is the essence of life; be willing to surrender what you are for what you could become.”
Real change starts with a careful assessment of what is not right with our life. The path toward change requires careful discernment in the context of our values, our relationships, what makes us feel content, and how a problem tangibly affects our day-to-day life. From this can emerge a carefully considered plan for a long-term change of course rather than a quick fix. Successful, real change is usually measured in months or years, through a series of innumerable small steps (and missteps).
When fully achieved, real change is a seismic movement of the soul, a visible expression of our values − what lies within our heart. With a sincere desire for change, as Sharon Salzberg notes “…. the engagement that results can be an openhearted demonstration of what we care about most deeply. Efforts toward change are an expression of our own innate dignity and testaments of the belief that what we do matters in this world. We engage not only to try to foster change right now − we engage to enliven what we believe to someday be possible.” In what Mary Oliver calls our “one wild and precious life,” we have been given many gifts, among them our sense of purpose, connection with others, grace, and an innate capacity for change − again and again − as we travel through this life in this world.
Brian Sayers, MD
Chair, TCMS Physician Wellness Program
Contact Dr. Sayers at briansayers24@gmail.com